So, you’ve made it through the first two years of medical school. Congratulations. You've spent countless hours buried in textbooks, memorizing biochemical pathways and anatomical structures. Now, it's time to step out of the lecture hall and into the real world of medicine. This is where the clerkship begins.
A clerkship is the pivotal moment you trade your textbooks for a stethoscope and start working with actual patients in hospitals and clinics. It's an intense, hands-on apprenticeship—usually starting in your third year—where all that theory you've learned finally gets put into practice under the watchful eye of experienced physicians.
The Bridge From Classroom to Clinic

This is the part of medical school that feels truly real. The first two years are all about building your scientific foundation from books and lectures. Clerkships flip that entire script. You're no longer just a student in a classroom; you're now an active, contributing member of a patient care team on the hospital wards.
Think of it as the ultimate learn-by-doing experience. Instead of just reading about symptoms, you'll be the one taking a patient's history. Instead of memorizing treatment algorithms, you'll be helping your team create and carry out a real patient's care plan.
The core purpose of a clerkship is to transform you from a student who knows about medicine into a student who practices medicine. It’s about building the bridge between information and application.
This isn't about shadowing from the sidelines. You're expected to be an active participant, and this hands-on involvement is absolutely essential. The entire experience is designed to build the foundational skills that you simply can't learn from a textbook.
Key Components of a Medical Clerkship at a Glance
To give you a clearer picture, this table breaks down the essential parts of the clerkship experience. It's a quick cheat sheet to what you'll be doing and why it's so important for your training.
| Component | Description | Primary Goal |
|---|---|---|
| Patient Interaction | Taking histories, performing physical exams, and presenting findings to the medical team. | Develop foundational clinical skills and build patient rapport. |
| Team Integration | Working alongside residents and attending physicians as a member of the healthcare team. | Understand team dynamics and learn to communicate effectively in a clinical setting. |
| Didactic Learning | Attending lectures, grand rounds, and case conferences specific to your current rotation. | Supplement hands-on experience with structured, specialty-specific knowledge. |
| Clinical Reasoning | Formulating differential diagnoses and contributing to the development of patient management plans. | Move from memorization to the practical application of medical knowledge. |
| Assessment | Evaluations from supervisors, standardized patient exams (OSCEs), and end-of-rotation shelf exams. | Measure clinical competency, knowledge retention, and professional growth. |
Each of these components works together to mold you into a thinking, feeling, and functioning future doctor.
Developing Core Clinical Abilities
During your clerkships, the main goal is to build the essential skills that form the bedrock of any competent physician. This goes way beyond just reciting medical facts. You’ll finally learn how to:
- Take a comprehensive patient history: This isn't just about running through a checklist. You'll learn the art of asking insightful questions that help you uncover the real story behind a patient's illness.
- Perform a thorough physical exam: You'll master the hands-on techniques needed to accurately assess a patient's physical condition, from listening to heart sounds to testing neurological reflexes.
- Present patient cases to a medical team: This means learning to communicate your findings, assessments, and plans clearly and concisely to your supervising residents and attending physicians. It's a skill you'll use every single day of your career.
- Formulate a differential diagnosis: This is where you really start thinking like a doctor. You'll learn to create a list of potential diagnoses for a patient's symptoms and then reason your way through them.
This entire process is designed to sharpen your mind and teach you how to improve critical thinking, a skill that’s vital for analyzing complex cases and making sound decisions. It marks the true beginning of your journey toward mastering what is clinical reasoning, the very heart of what it means to be a physician.
Navigating Your Core Medical School Rotations
Your third year is where the rubber meets the road. It’s structured around a series of core rotations—required, multi-week dives into the foundational specialties of medicine. Think of it as a guided tour through the hospital's major departments, where you get a concentrated dose of experience in one field before moving on to the next.
This isn’t just about checking boxes. The whole point is to give you a broad, practical understanding of the entire medical landscape. You’ll spend time in the high-stakes world of the operating room, the cerebral environment of internal medicine wards, and the unique settings of pediatrics and psychiatry. It's all designed to build a solid, versatile foundation, no matter which specialty you ultimately fall in love with.
The Six Pillars of Your Clerkship Year
Most U.S. medical schools build their third year around six fundamental specialties. The order and length might differ from one program to another, but you can count on completing a dedicated clerkship in each of these core areas.
- Internal Medicine: This is often seen as the backbone of hospital care. You'll focus on diagnosing and managing complex illnesses in adult patients.
- Surgery: A hands-on rotation where you’ll scrub in, learn sterile technique, assist in the OR, and manage patients both before and after their procedures.
- Pediatrics: Get ready to cover the full spectrum of child health, from checking newborns to navigating adolescent medicine.
- Obstetrics & Gynecology (OB/GYN): A dynamic field centered on female reproductive health, pregnancy, and childbirth. To keep up, you'll need to master a unique knowledge base, and our detailed OB/GYN shelf review can give you the focused prep you need.
- Psychiatry: Here, you'll learn to diagnose and treat mental health conditions, with a heavy emphasis on the patient interview and therapeutic communication.
- Family Medicine: This rotation offers a window into primary care, highlighting continuity of care for patients of all ages, usually in an outpatient clinic.
An Evolving Educational Model
The traditional structure of medical education is shifting. More and more, schools are weaving clinical experience into the curriculum much earlier to make sure students are better prepared for the realities of patient care.
This reflects a broader trend to ensure students get meaningful patient exposure sooner rather than later. The timing of clerkships has changed dramatically over just the past couple of decades.
Take the neurology clerkship, for example. Research from the American Academy of Neurology shows that in 2005, a staggering 45.6% of these clerkships were only taken in the fourth year. Fast forward to 2022, and that number plummeted to just 3%. It’s a clear sign that medical schools are redesigning their programs to create a more logical and effective learning path.
Each rotation you complete will throw a distinct set of challenges and learning opportunities your way. From the procedural skills you’ll pick up in surgery to the long-term patient relationships you’ll build in family medicine, this year is all about shaping you into a well-rounded physician.
A Day in the Life on the Wards
The jump from the classroom to the wards is probably one of the most jarring transitions in medical school. One day you're in lectures, and the next, you're an active member of a medical team. The days get longer, the learning curve feels vertical, and everything is driven by the urgent needs of patients, not a syllabus.
So what does a day really look like? Let's walk through a typical schedule on a busy rotation like surgery or internal medicine to get a real feel for it.
Your alarm will likely go off before the sun is up. While most of the world is still asleep, you’re already at the hospital, getting ready for "pre-rounds." This is your solo mission to check in on your assigned patients, see how they did overnight, comb through nursing notes, and review any new lab results that came in. The goal is to be the expert on your patients before the rest of the team even arrives.
From Pre-Rounds to Patient Presentations
Once the residents and the attending physician show up, it's time for official "rounds." This is showtime. You'll present each of your patients in a clear, structured way, covering their overnight progress and laying out your assessment and plan for the day. It’s definitely a high-pressure moment, but it’s also where you sharpen your clinical reasoning and learn to communicate like a physician.
The hospital is a fast-paced, team-based environment, and your ability to work with others is critical. Knowing how to improve team communication isn't just a soft skill—it directly impacts how well you perform and, more importantly, patient safety.
After rounds, the "real" work begins, and it looks different depending on where you are:
- On Surgery: You could spend your entire day in the operating room. You'll be scrubbing in, holding retractors, learning to suture, and watching incredible procedures up close.
- On Internal Medicine: You’ll be on the floor managing your patients. This means writing notes, putting in orders for tests, calling consults, and handling new admissions or discharges.
- In Clinic: On an outpatient rotation, you'll see a steady stream of scheduled patients. You’ll take their history, perform a physical exam, and then present your findings to the attending before they go in.
The Second Shift: Studying After Hours
Just because you leave the hospital doesn’t mean your day is over. For many, the clinical day rolls right into the late afternoon or evening, and that’s when your second job starts: studying for the shelf exam. This constant juggle is easily one of the biggest shocks of clerkship year.
You’re essentially working a full-time job while studying for some of the most challenging exams in your medical career. It’s a grind that demands a whole new level of discipline.
Figuring out a study rhythm that works is absolutely crucial. So many students feel like they're drowning, but it's completely possible to succeed with a smart strategy. For some practical advice, our guide on how to study for Step 2 CK during clinical rotations has tips that work just as well for shelf prep. The resilience you build during this intense time will stick with you for the rest of your career.
How You Are Graded in Clinical Rotations
Understanding how you're graded during clerkships is just as important as the clinical work itself. This isn't like your preclinical years where everything boiled down to a single exam score. Rotations are different. Your grade is a blend of subjective feedback, standardized tests, and hands-on performance.
Your final grade for each rotation is a composite score pieced together from three distinct areas. Each one is designed to test a different part of your competence—from your bedside manner and teamwork to your raw medical knowledge. Getting a handle on this system is the key to thriving, not just surviving.
The Three Pillars of Your Clerkship Grade
Think of your evaluation as a three-legged stool. It rests on a trio of assessments, and each one carries a lot of weight. If you knock it out of the park in one area, it can help balance a weaker performance in another, but the real goal is to be solid across all three.
- Clinical Evaluations: This is the subjective piece of the puzzle. The attending physicians and residents you work with day in and day out will be evaluating you. They're looking at your professionalism, how well you integrate into the team, your clinical reasoning, and the way you interact with patients.
- NBME Shelf Exam: At the very end of each rotation, you'll sit for a standardized multiple-choice exam created by the National Board of Medical Examiners (NBME). This is a high-stakes test designed to assess your foundational knowledge in that specific specialty, like Surgery or Pediatrics.
- Objective Structured Clinical Examination (OSCE): This is your practical, hands-on exam. You'll move through different stations with standardized patients (actors trained to portray a specific case) where you're graded on your ability to take a history, perform a physical exam, and communicate your findings and plan effectively.
This flowchart breaks down what a typical day might look like, and you can see how all these daily activities feed directly into your final evaluations.
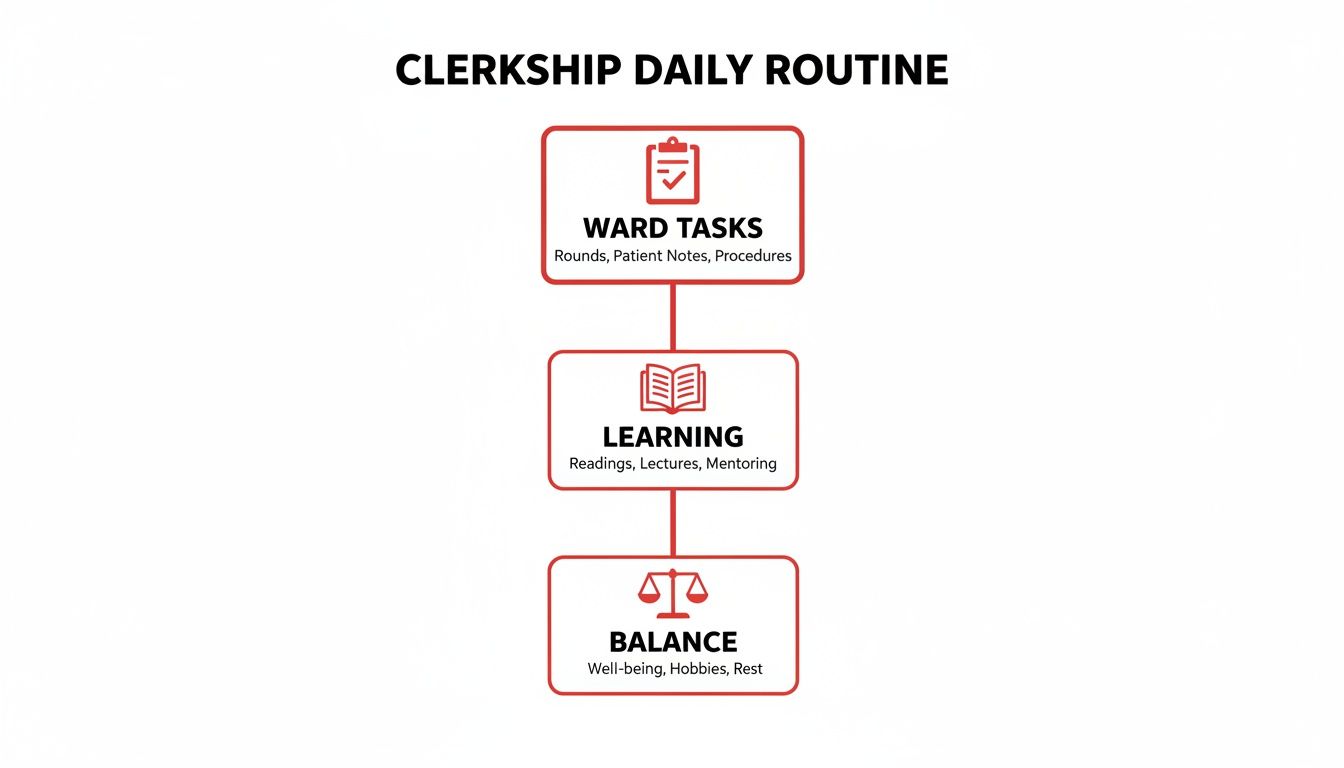
It really highlights the constant juggling act between handling your responsibilities on the wards, carving out time for dedicated study, and just trying to stay sane—all of which are critical for a strong performance.
The Critical Role of the Shelf Exam
While your performance on the wards is hugely important, the Shelf exam often acts as the great equalizer. It’s an objective, standardized yardstick that residency program directors can use to compare you to applicants from every other medical school in the country.
A strong performance on your Shelf exams is one of the most effective ways to stand out, especially in a system where clinical grades can be inflated.
This is more true now than ever. Grade inflation in clerkships has become a real issue, with the number of "Honors" grades climbing every year. For instance, between 2019 and 2022, the average percentage of honors grades in surgery clerkships jumped from 34.6% to 38.6%. When nearly everyone is getting top marks, your Shelf score provides the hard data needed to prove you’ve truly mastered the material.
These exams aren't just hoops to jump through, either. They are direct preparation for the USMLE Step 2 CK. The questions are written in the exact same style and cover the same high-yield content you'll see on your boards. The best way to prepare is to grind through question banks and get comfortable with the test format.
If you're looking for an edge, digging into resources on NBME practice shelf exams can give you a much-needed structured approach. In the end, your Shelf scores, clinical evaluations, and OSCE performance all come together to paint a complete picture of your readiness for the next stage of your medical career.
Proven Strategies to Excel During Clerkship

The clerkship year is a constant balancing act. You're juggling long hours on the wards with the ever-present need to study for your next Shelf exam. Thriving here means mastering both sides of that coin.
On the floor, your job is simple: become a valuable, indispensable part of the team. That means showing up early, being willing to stay late, and always bringing a proactive attitude. Genuine curiosity about your patients will take you far.
Don't wait for your residents to hand you a to-do list. Actively look for ways to lighten their load. Offer to call that consult, track down that missing lab result, or get a head start on patient notes. This kind of initiative gets you noticed for all the right reasons and heavily influences your final grade.
The secret to a strong clinical evaluation isn't just knowing the right answers; it's being the student who consistently makes the team's job easier. Reliability and a positive attitude are just as important as your medical knowledge.
Building this reputation is foundational. It opens the door to better teaching moments from your attendings and will be crucial when you need strong letters of recommendation for residency.
Mastering Your Clinical Performance
Everything you do on the wards is being observed. To make a lasting, positive impression, zero in on these key areas.
- Own Your Patients: You need to be the absolute expert on the patients you're following. Be ready to present their overnight events, morning labs, and the clinical reasoning behind their current treatment plan without fumbling through your notes.
- Refine Your Presentations: Nobody has time for a rambling, disorganized presentation. Practice delivering your patient summaries in a clear, concise, and structured way. It shows you respect your team's time and have a solid grasp of clinical reasoning.
- Ask Insightful Questions: Avoid asking questions that a quick Google search could answer. Instead, ask the "why" questions that dig into clinical decision-making. For example, "Why did we choose this antibiotic over another for this patient's specific comorbidities?"
These actions signal that you're thinking critically about patient care, not just checking boxes. It shows you're an active learner, not a passive observer.
Developing a Sustainable Study Plan
While you’re putting in the hours on the wards, that Shelf exam is always just around the corner. Success demands an efficient, consistent study plan that won’t lead to total burnout. Your time is too limited to waste on low-yield resources.
The key is to weave studying into the fabric of your day. Use that downtime between rounds to knock out a few practice questions on your phone. Listen to a relevant medical podcast on your commute. Instead of trying to cram everything into the weekend, aim for a manageable number of questions each night. This approach uses spaced repetition and active recall—two methods proven to boost long-term retention.
For a deeper dive into building an effective schedule, our complete guide to shelf exam preparation offers a detailed roadmap for balancing your clinical duties with high-yield learning.
Remember, the goal of clerkship is to build a rock-solid foundation for your future as a physician. By excelling both in the clinic and on your exams, you're setting yourself up for success on your boards and in your residency applications.
Overcoming the Clerkship Scarcity Challenge
Let's be honest: finding a truly high-quality clerkship has gotten tough. It’s a simple numbers problem—medical school enrollment has exploded, but the number of clinical training sites and physicians willing to teach hasn't kept pace.
This isn’t just an administrative headache; it has real-world consequences for you. You might land in a rotation with less one-on-one supervision, fewer chances to get your hands on actual procedures, or find yourself competing with five other learners for a single attending's attention. It puts the responsibility squarely on your shoulders to drive your own education.
The challenge isn't just about finding a spot anymore. It's about squeezing a meaningful educational experience out of the spot you get. Your ability to adapt and actively hunt for learning opportunities is more critical than ever.
This new reality means you have to walk into every single rotation with a proactive game plan. Even in a crowded or less-than-perfect setting, you have the power to create an outstanding learning experience for yourself.
Proactive Strategies for Thriving in Any Rotation
At its core, this is a classic supply-and-demand imbalance. An eye-opening report from the Association of American Medical Colleges (AAMC) revealed that 84% of medical school deans are worried about the number of available clerkship sites. This issue was supercharged by a 33% spike in U.S. medical school enrollment between 2002 and 2019, which pushed the system to its limits. Exploring the data on this trend really puts the scope of the problem into perspective.
So, how do you make the most of your clerkships despite these hurdles? Focus on what you can actually control.
- State Your Goals on Day One: Don't be shy. On your first day, tell your residents and attending what you specifically hope to get out of the rotation. "I'd really like to get better at presenting patients" or "I'm hoping to practice my suturing skills" goes a long way.
- Show Unwavering Initiative: The worst thing you can do is stand in a corner waiting for an assignment. Volunteer to see the new admission. Offer to write the note. Ask if you can help with a procedure, even if it's just holding a retractor. A student who actively looks for work is a student who gets noticed.
- Build Your Network: Make friends with everyone—the residents, the nurses, the respiratory therapists. They are walking encyclopedias of practical knowledge and are often the ones who will flag you down for a cool learning opportunity that you would have otherwise missed.
- Master the "Why": Show up to the wards prepared. If your patient has pancreatitis, you should have a solid grasp of the pathophysiology before rounds. This not only shows you're engaged but makes clinical discussions ten times more productive and impressive.
Common Questions About Medical Clerkships
Even after getting the big picture, most students have a few lingering practical questions as they gear up for this intense year. Let's tackle some of the most common ones.
How Do I Choose Elective Rotations in My Fourth Year?
Think of your fourth-year electives as a strategic campaign to lock in your residency spot. The goal is twofold: secure powerful letters of recommendation in your chosen specialty and explore sub-specialties that genuinely excite you.
The most critical pieces of this puzzle are your "audition" rotations, also known as sub-internships (or Sub-Is). Scheduling these at programs high on your rank list is non-negotiable. They are your chance to make a direct, lasting impression on the faculty and, just as importantly, to see if the program’s culture is a place where you'll thrive.
What Is the Difference Between a Clerkship and a Sub-Internship?
A core clerkship in your third year is your formal introduction to a specialty. You're there primarily as a student, learning the ropes and absorbing as much as possible.
A sub-internship (Sub-I), which you'll do in your fourth year, is a whole different ballgame. It’s an advanced rotation where you step into the shoes of an intern.
During a Sub-I, you are expected to carry more patients, write the primary notes, and take first call under supervision. It serves as the ultimate test to prove you are ready for the demands of residency.
Think of it this way: a clerkship is like learning to drive with an instructor who has their own set of brakes. A Sub-I is when they hand you the keys for your first solo drive on the highway.
Can I Do Clerkships Internationally?
Absolutely, and many medical schools offer fantastic opportunities for international rotations, almost always as fourth-year electives. These experiences can be incredible for personal growth, giving you a valuable, firsthand look at global health challenges and entirely different healthcare systems.
However, a word of caution: you need to balance this with your domestic goals. Residency program directors in the U.S. place a huge premium on strong clinical performance within the U.S. healthcare system.
So, by all means, explore an international rotation if it’s well-structured and approved by your school. Just don't let it take the place of those essential sub-internships back home that will directly impact your residency match.
Navigating the complexities of clerkships, shelf exams, and residency applications can be overwhelming. Ace Med Boards offers personalized, one-on-one tutoring to help you excel on your shelf exams and boards, ensuring you stand out. Learn more about our expert guidance at https://acemedboards.com.
