The Computer-based Case Simulations (CCS) portion of Step 3 isn't just another section on the exam—it’s a completely different beast. Your success with step 3 ccs cases comes down to mastering the clunky software and adopting the specific, almost algorithmic, approach the USMLE rewards. You have to shift from your real-world clinical instincts to a more structured, point-scoring mindset.
Let's break down exactly what the simulation is designed to test.
Decoding The CCS Case Simulation
The biggest mistake I see residents make is treating a CCS case like a real patient. It’s not. It’s a performance designed to test specific skills in a controlled, artificial environment.
The software isn't looking for diagnostic brilliance alone. It's grading your systematic process, your thoroughness, and your ability to manage a patient from start to finish within a simulated timeline. This means simple actions you take for granted in the hospital—like making a patient NPO or ordering IV access—are discrete, point-scoring opportunities you absolutely cannot afford to miss.
At its core, a CCS case is one of the many skills assessment tests you'll encounter, just wrapped in a clinical scenario.
Core Competencies Under The Microscope
The simulation is grading several key areas at once. Nailing the focused history and physical is just the ticket to entry. The real test is how you use that initial data to build a differential and then formulate a solid diagnostic plan.
So, what are they actually looking for?
- Initial Orders: Did you remember the basics on an acutely ill patient? Think vital signs, IV access, and baseline labs like a CBC and BMP.
- Time Management: Are you advancing the clock logically to check on results, or are you letting the patient languish in the virtual ED for hours with no follow-up?
- Reassessment: After giving a medication or getting labs back, did you re-evaluate the patient's status and tweak your plan? You have to show you're responsive.
- Patient Disposition: Do you know when to move the patient? This means correctly transitioning them from the clinic to the ED, or from the ED to an inpatient floor, at the appropriate time.
This flow chart gives you a great visual of how a typical case should progress, from the initial workup to the final disposition.
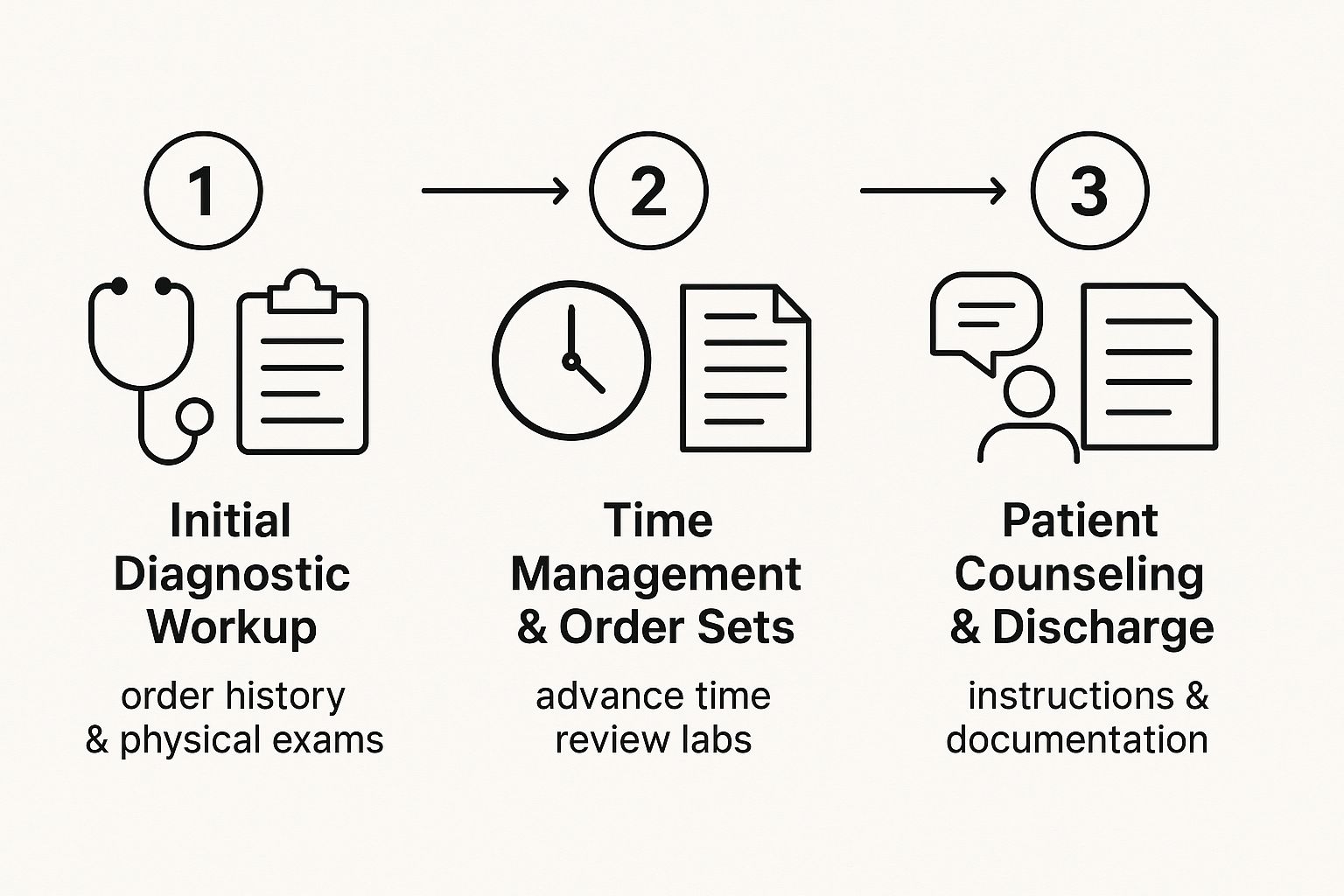
It really highlights that success isn't about one single brilliant move. It’s a chain of logical, sequential decisions. If you forget a crucial step, like counseling a patient on smoking cessation before discharge, you break that chain and lose easy points.
The Mindset Shift From Clinic To Simulation
In the hospital, you rely on gestalt, verbal orders, and the help of your team. In the CCS world, none of that exists. If you don't type it into an order, it simply didn't happen. Every single action, from ordering Tylenol for a headache to providing discharge instructions, must be explicitly entered into the system.
For a full rundown of all the topics you might encounter, it’s a good idea to review the complete https://acemedboards.com/usmle-content-outline/ to get a feel for the scope.
To succeed, you have to make a critical mindset shift. It's not about being the most efficient real-world doctor; it's about being the most thorough, methodical doctor according to the exam's rigid rules. This table breaks down some of the key differences.
Key Differences Between Real Clinic and CCS Cases
| Clinical Aspect | Real-World Practice | CCS Case Strategy |
|---|---|---|
| Ordering | Often relies on verbal orders, protocols, and team support. | Every single action must be explicitly typed and ordered. If it's not documented, it didn't happen. |
| Pacing | Driven by patient acuity and hospital workflow. | Driven by advancing the clock to see results and make sequential decisions. Inaction is penalized. |
| Thoroughness | Efficiency is key; you focus on the most likely diagnosis. | Be overly systematic. Order broad labs and consults to prove you considered a wide differential. |
| Counseling | Often happens organically during patient conversations. | Must be entered as a specific, discrete order (e.g., "Counsel patient – smoking cessation"). |
| Patient Status | You might assume a patient is NPO or has IV access. | You must explicitly order "NPO," "IV access," "Oxygen," and "Continuous monitoring." |
This table underscores the need to be deliberate and almost robotic in your approach. You have to prove to the computer that you're a safe and systematic physician.
The crucial insight is this: The USMLE Step 3 CCS cases reward systematic, thorough, and sometimes redundant-feeling actions. The goal is to prove you are a safe and methodical physician according to their specific rubric, not necessarily the most efficient one in a real-world setting.
Your Strategy for the First Two Minutes

How you begin a CCS case almost always determines your final score. The first 120 seconds are your golden window to establish control, pull in critical data, and get ahead of the clock. A shaky, disorganized start can easily snowball into missed steps and lost points, but a systematic approach builds the momentum you need to crush the case.
Think of it like running a code in real life. You have an immediate, almost reflexive, set of actions for an unstable patient before you even know the underlying cause. The same exact logic applies here. You need a battle-tested routine that you can execute flawlessly the moment a new case pops up on your screen. This isn't about rushing; it’s about being efficient and deliberate.
Your Immediate Action Plan
The second you read the initial patient vignette, your first job is to figure out the setting and the patient's stability. Is this a chill outpatient clinic visit for a chronic issue, or are you in the ED with someone in acute distress? That initial read guides your entire first wave of orders.
For any patient showing up in an emergency setting, your initial moves should be automatic. Don't waste precious seconds trying to nail the diagnosis just yet. Focus on stabilization and data collection. These foundational steps are almost always correct and rack up easy points.
Here’s a practical checklist for that first critical minute:
- Vitals & Monitors: The very first thing you should always order is a full set of vital signs. Immediately follow this with continuous cardiac monitoring and pulse oximetry. These are separate orders on the system, and it's a super common mistake to forget one.
- Safety Net Orders: Get that IV access established. Order oxygen, usually starting with a nasal cannula. Make the patient NPO (nil per os) if they have any abdominal pain, altered mental status, or any chance of needing surgery.
- Initial Physical Exam: Perform a focused physical exam based on the chief complaint. For chest pain, that means a thorough cardiovascular and pulmonary exam. For a headache, you absolutely need to include a full neurological assessment.
This initial volley of orders ensures your patient is safe and starts feeding you the baseline data you need to build your differential diagnosis. You're essentially creating a safety net while you think.
Ordering Your First Wave Of Labs
Once you've secured the patient and ordered monitors, your next immediate step is to order a broad but logical panel of labs. In the world of Step 3 CCS cases, casting a slightly wider net at the beginning is rewarded. It shows the graders that you're thinking through a broad differential.
For a typical, undifferentiated patient in the emergency department, your initial lab set should look something like this:
- Core Bloodwork: Complete Blood Count (CBC) with differential, Basic Metabolic Panel (BMP), and Liver Function Tests (LFTs).
- Coagulation Studies: Prothrombin Time (PT), International Normalized Ratio (INR), and Partial Thromboplastin Time (PTT).
- Cardiac Markers: Troponin is a must if there's any mention of chest pain, shortness of breath, or cardiac risk factors.
- Key Screenings: Urinalysis and a urine pregnancy test (beta-hCG) for all female patients of childbearing age, no matter what they came in for. Don't skip this.
A critical takeaway for the first two minutes is to prioritize stabilization and broad data gathering over a specific diagnosis. Ordering IV access, oxygen, monitors, and a standard set of labs for any acutely ill patient is a universal strategy that prevents early mistakes and builds a strong foundation for the rest of the case.
Once these initial orders are in, you can take a breath and review the history provided. As you advance the clock, the results from your physical exam and these initial labs will start rolling in. This is the information that lets you pivot from a broad, shotgun approach to a much more focused diagnostic workup. Mastering this two-minute drill turns panic into a repeatable, point-scoring process for every single case.
Mastering the Clock and Your Order Sets

Time management is the hidden skill that separates a good score from a great score on Step 3 CCS cases. This isn't about raw speed; it's about making deliberate, efficient moves that push the case forward.
Think of yourself as a director. You control when the scene changes. Advance the clock too far, and you risk the patient deteriorating while you miss crucial interventions. Advance it too little, and you're just sitting there, burning valuable time. The art lies in advancing time just enough to get critical results back.
Your goal is to find a rhythm: place orders, advance the clock to get the results, pause to interpret the new data, and then act on it. This simple loop—order, advance, assess, act—is the fundamental engine of every successful CCS case.
Building Logical Order Sets
When a case kicks off, your initial orders should be broad enough to cover your bases. But as the clinical picture sharpens with incoming lab and imaging results, your order sets must become more specific and targeted. Wasting time and resources on unnecessary tests is a classic way to lose points.
Let's take a patient presenting with altered mental status. Your first wave of orders is intentionally wide:
- Initial Labs: CBC, BMP, LFTs, TSH, ammonia, toxicology screen, urinalysis.
- Imaging: A non-contrast head CT to rule out an acute bleed is a must.
- Safety Measures: IV access, continuous monitoring, and maybe a quick fingerstick glucose at the bedside.
Now, imagine the initial results start rolling in. The head CT is clean, but the BMP flags a sodium of 118 mEq/L. Suddenly, your focus shifts. Your next set of orders becomes laser-focused on diagnosing and managing the hyponatremia. You'll order serum and urine osmolality, urine sodium, and start thinking about fluid restriction or hypertonic saline depending on the patient's stability.
You've successfully narrowed your workup from a broad differential to a specific, manageable problem. That’s the game.
The Art of Advancing Time Strategically
The "Advance Clock" function is your most powerful tool, and the key is almost always selecting "to time of next available result." This simple choice prevents you from jumping hours ahead and missing a critical update that just came back.
The single biggest time management mistake is advancing the clock by a fixed interval like "1 hour" or "4 hours." This is a total gamble. Instead, let the simulation guide you. Advancing to the next piece of information ensures you never miss a chance to react to new data as it arrives.
For example, in a classic chest pain case, after ordering an EKG, troponins, and a chest X-ray, you should immediately advance to the next available result. The EKG will likely be back first. This allows you to react to it—maybe by giving aspirin and nitroglycerin—before the troponin result is even available. This step-by-step approach shows the graders you're responsive and methodical, not just waiting around.
Don't Forget the Easy Points: Follow-Ups and Counseling
So many test-takers get tunnel vision on the acute problem that they completely forget the "wrap-up" points that signal comprehensive care. These are easy points, and they’re often left on the table.
After you've stabilized the patient and locked in the diagnosis, you must schedule two final things before ending the case:
- A Follow-up Appointment: Always, always schedule a follow-up visit. This shows you’re thinking about the patient's long-term care and ensuring continuity.
- Patient Counseling: This is a huge point-scorer. You must explicitly order counseling for relevant issues. Think smoking cessation, medication adherence, diet, or education on their new diagnosis. If you don't type it in as an order, it didn't happen.
Effectively managing your time and sequencing your orders is a skill that only comes with practice. Weaving dedicated case practice into your routine is essential, and building a structured plan can make all the difference. To help with this, check out our guide on creating an effective Step 3 study schedule that perfectly balances CCS practice with your MCQ review.
Navigating Common CCS Case Traps

It’s one thing to know the right moves in step 3 ccs cases; it's another to execute them flawlessly with the clock ticking. The biggest threat to your score isn't a knowledge gap—it's the unforced errors. These are simple mistakes in process, usually born from panic, tunnel vision, or just forgetting the unique rules of the simulation.
The key to a high score is recognizing these traps before you fall into them. When you know what the common pitfalls look like, you can build a systematic defense against them. This ensures your hard-earned clinical knowledge actually translates into points on the board. Let's break down the most frequent mistakes I've seen and, more importantly, how to sidestep them.
The Over-Ordering Avalanche
When a diagnosis isn't immediately obvious, the urge to order every test under the sun is strong. It feels like a safe, "shotgun" approach, but the CCS software is designed to penalize this exact behavior. Ordering an invasive or expensive test too early—like jumping to a V/Q scan before a D-dimer in a low-risk patient—will absolutely cost you points.
The secret is sequential ordering. You have to think like a real-world clinician managing resources. Start with the least invasive, highest-yield tests first. For instance, in a patient presenting with abdominal pain, you wouldn’t go straight for a HIDA scan. A logical sequence looks something like this:
- Initial Labs: Get the basics first. A CBC, BMP, LFTs, and lipase will give you a ton of information.
- Basic Imaging: An abdominal ultrasound is fast, non-invasive, and the perfect first step for RUQ pain.
- Advanced Imaging: Only after those initial tests point toward a specific pathology (like cholecystitis) should you order a more specific test like a HIDA scan.
This tiered approach shows the computer you have sound clinical reasoning, which is precisely what the test is designed to measure.
The "Fire and Forget" Fumble
This one is painfully common. You order a critical intervention and then move on without checking if it actually worked. You gave albuterol for an asthma attack—great. But did you go back and re-examine the patient’s lungs? Did you check a repeat peak flow? If not, the system assumes you weren't monitoring your patient's response to treatment.
After every significant action—whether it’s giving a fluid bolus, administering a medication, or changing the oxygen level—you must advance the clock a few minutes and re-evaluate. This demonstrates a closed-loop thought process: intervene, assess the result, and then decide the next step.
Failing to do this is one of the easiest ways to bleed points. You have to explicitly show the software that you’re paying attention. A simple "Physical Exam – Lungs" after a breathing treatment can make all the difference in your score.
Neglecting the Endgame Points
So many test-takers get completely wrapped up in the diagnosis and acute treatment that they forget the final, crucial steps of the encounter. Ending a case without the proper disposition and counseling is like running a marathon and stopping one foot short of the finish line.
You have to remember these critical "endgame" orders to squeeze every last point out of a case:
- Patient Counseling: This is a goldmine for easy points. Always order counseling on relevant topics like smoking cessation, medication adherence, diet changes, or education on their new diagnosis.
- Follow-Up: A patient is never discharged into the void. Make sure you schedule a follow-up appointment, whether it's with their PCP in a week or a specialist in a month.
- Disposition: The case won't end until you decide where the patient goes. If they're stable, order "Discharge Home." If they need admission, transfer them to the appropriate floor.
These actions demonstrate that you’re not just a diagnostician but a complete physician who thinks about the entire continuum of care. This comprehensive view is valued everywhere. In fact, the broader Carbon Capture and Storage (CCS) market has seen massive growth by addressing the full lifecycle of a process. In 2024, the global CCS market hit an estimated value of USD 8.6 billion, with forecasts showing a significant 16% compound annual growth rate through 2034. You can learn more about these market growth findings to see how this expanding field operates. Mastering the full scope of your step 3 ccs cases, just like in industry, is what leads to real success.
Building Your Personal Practice Plan
Mastering the CCS portion of Step 3 isn’t about passively absorbing information—it's about building a skill. You need to develop the muscle memory to navigate that clunky software and execute a systematic plan, all while the clock is ticking. A structured approach is what turns this intimidating task into a manageable, point-scoring part of your study routine.
Let's be clear: you can't just read about strategies and expect to succeed. The only way to get comfortable with the unique rhythm of step 3 ccs cases—placing orders, advancing time, and reassessing data—is by getting your hands dirty and doing it over and over again. This is how you build the confidence and efficiency you'll need on the actual exam day.
Choosing Your Practice Resources
Your main goal here is to simulate the real test environment as closely as humanly possible. While there are a bunch of resources out there, a few stand out as essential. It's far better to focus your energy on one or two top-tier tools rather than spreading yourself too thin.
Here’s a breakdown of the most effective resources available:
- UWorld CCS: This is, without a doubt, the gold standard. Its interface is a near-perfect mimic of the real exam, and its library of cases covers the high-yield scenarios you're almost guaranteed to encounter. The detailed feedback you get after each case is invaluable for seeing where you went wrong and understanding the scoring logic.
- Official USMLE Practice Materials: The NBME provides free practice cases directly on its website. The number of cases is limited, but working through them is non-negotiable. This is the only way to get a true feel for the software and question style straight from the source.
- Other Q-banks: Some other test prep companies offer their own CCS case simulations. These can be useful for extra practice if you've already burned through UWorld and the official materials, but always prioritize the resources that most accurately reflect the real exam.
The most effective study plan centers on active practice with a tool that mimics the real exam software. Prioritize completing every UWorld CCS case and all official USMLE practice materials, as this combination provides the most realistic and comprehensive preparation available.
Structuring Your Practice Timeline
Don't save all your CCS practice for the last week—that's a recipe for disaster. You need to weave it into your overall Step 3 study plan from the beginning. The goal is to build your skills gradually so the entire process feels second nature by the time you sit for the exam.
Start by just getting your feet wet. The first few cases will feel awkward and slow, and that’s completely normal. Your only objective at the start is to figure out how to place orders, perform a physical exam, and advance the clock without panicking.
Once you have the basics down, a "case-a-day" approach works wonders. Spending just 15-20 minutes each day on a single case is far more effective than trying to cram for hours on the weekend. This consistent, low-dose exposure helps solidify the core mechanics and keeps the concepts fresh.
The Power of Active Review
Just clicking through cases is only half the battle. The real learning happens when you actively review your performance. After every single practice case, you need to dissect what you did right and, more importantly, what you did wrong.
Ask yourself these critical questions during your review:
- Did I miss any of the initial "safety net" orders? Think IV access, O2, monitors, NPO status.
- Was my diagnostic workup logical and sequential? Or did I jump the gun and order an invasive test too early?
- Did I remember to re-evaluate the patient after each major intervention or time advance?
- Did I forget the crucial "endgame" points? This includes counseling, arranging follow-up, and setting the final disposition.
This kind of reflective process is what turns mistakes into learning opportunities. For a deeper dive into effective study habits and question analysis, check out our guide on tackling USMLE Step 3 practice questions. To really structure this learning, applying general knowledge management best practices can also provide a useful framework for organizing all the information you're taking in.
By systematically reviewing your performance, you'll start to spot recurring patterns in your approach. This allows you to refine your strategy, much like experts in any field analyze data to improve outcomes, ensuring you capture every possible point on exam day.
Answering Your Top CCS Case Questions
Even with a solid game plan, you're going to hit some weird snags during those late-night study sessions. The unique format of Step 3 CCS cases has a way of creating doubt around the little details of case management that just don't feel like real-world medicine.
Let's clear up some of that confusion right now. We'll tackle the most common questions that pop up when you're deep in the trenches of practice, because getting straight answers can make a huge difference on exam day.
How Do I Know When a Case Is Ending?
This is a classic source of anxiety. You've diagnosed the patient, started treatment, and they're getting better. Now what? You can't just walk away; you have to actively signal to the software that you're done.
A case is ready to end when two things have happened:
- You’ve solved the main clinical problem and the patient is stable.
- You’ve placed all the final disposition and follow-up orders.
The two-minute warning screen is your biggest clue here. When that pops up, it’s your final call to wrap things up. This is not the time to start a new, complex workup. Instead, shift your focus to the finishing touches. Make sure your patient has a follow-up appointment, you've provided all the necessary patient counseling (a goldmine for easy points), and you've officially entered the disposition order, like "Discharge Home" or "Transfer to Ward."
What If I Make a Big Mistake Early On?
Everyone has that moment of pure panic. You forgot to order a beta-hCG on a female with abdominal pain, or maybe you picked the wrong initial antibiotic. Take a deep breath. The good news is that the scoring is cumulative. A single error, especially one you catch and fix, isn't going to torpedo your entire score.
The key is how you recover. As soon as you realize your mistake, correct it. Forgot the pregnancy test? Order it now. See a lab result that makes your initial treatment look wrong? Change course. The simulation is testing your ability to reassess and adapt to new information—that's a core competency.
The CCS scoring system actually rewards you for correcting mistakes. Realizing you messed up and then fixing it shows better clinical judgment than just ignoring the error. Don't panic; just pivot.
How Should I Handle a Patient Who Leaves AMA?
Sooner or later, you'll get a case where a patient refuses treatment or wants to leave Against Medical Advice (AMA). This isn't a curveball; it's a test of your communication and documentation skills.
There’s a clear, point-scoring sequence you should follow every time:
- Counsel the Patient: Your first move is to order "Counsel patient – risks of leaving AMA" and explain what could happen if they leave.
- Assess Capacity: Briefly document that the patient is capable of making this decision (e.g., they are alert, oriented, and understand the risks you just explained).
- Offer Alternatives: See if you can propose a less intensive treatment plan they might agree to.
- Document Everything: Write a quick, concise patient note that summarizes the whole discussion.
- Provide Prescriptions & Follow-up: Give them any necessary prescriptions and crystal-clear instructions on when they need to return to the ED or see a doctor.
Nailing these steps shows you can handle a tough situation safely and professionally.
Should I Order Consults?
Yes, but do it with purpose. Ordering a consult (e.g., "Consult – General Surgery") is the right move once you have a clear reason to bring in a specialist. For a classic appendicitis case, you should consult surgery right after your initial workup—labs and imaging—points strongly to that diagnosis.
Just remember, consults in the CCS simulation are a one-way street. You will not get any recommendations back. The software gives you points just for ordering the consult at the right time because it shows you know when to call for help.
Don't sit around waiting for a reply that will never come. Continue managing the patient with appropriate orders like IV fluids, antibiotics, and pain control while you "wait" for the surgical team. Think of it as checking a box at the correct point in your management plan.
Navigating the nuances of Step 3 CCS cases is a skill built through practice and expert insight. If you're looking for personalized strategies to master these simulations and maximize your score, Ace Med Boards offers one-on-one tutoring designed for your specific needs. Visit us at https://acemedboards.com to schedule a free consultation and get the confidence you need to excel.
