The residency interview is a two-way street. While programs are evaluating your qualifications, it's your critical opportunity to assess their suitability for your career aspirations and personal well-being. Asking the right questions to ask residency programs goes far beyond demonstrating simple interest; it's a strategic process of discovery. You are gathering the essential data needed to determine where you will not just survive, but truly thrive for the next several years. A program's website can tell you about its structure, but it rarely reveals the nuances of its culture, the reality of its support systems, or the true nature of its educational philosophy.
This comprehensive guide moves past the generic and dives into eight critical categories of questions. These are designed to give you a clear, honest picture of what your life as a resident will actually be like day-to-day. Each question is a key that can unlock vital information, helping you differentiate between programs that look similar on paper. Preparing a list of thoughtful inquiries is essential, and to help you formulate even more personalized and insightful questions, consider using a tool like an Interview Question Generator to tailor your approach.
Making this decision requires more than just gut feelings; it demands concrete information. By asking targeted, specific questions, you can move from a superficial understanding to a deep, practical knowledge of each program. This approach will empower you to make one of the most important decisions of your medical career with confidence and clarity, ensuring you secure a position that aligns perfectly with your long-term personal and professional goals.
1. What is the training curriculum and how is it structured?
Beyond the program's reputation or location, the curriculum is the very foundation of your training for the next three to seven years. This is one of the most fundamental questions to ask residency programs because it directly impacts your day-to-day experience, skill acquisition, and preparation for your future career, whether in academic medicine, private practice, or a fellowship. The structure of clinical rotations, didactic learning, and hands-on training varies significantly between institutions, and finding the right fit is crucial for your success and well-being.
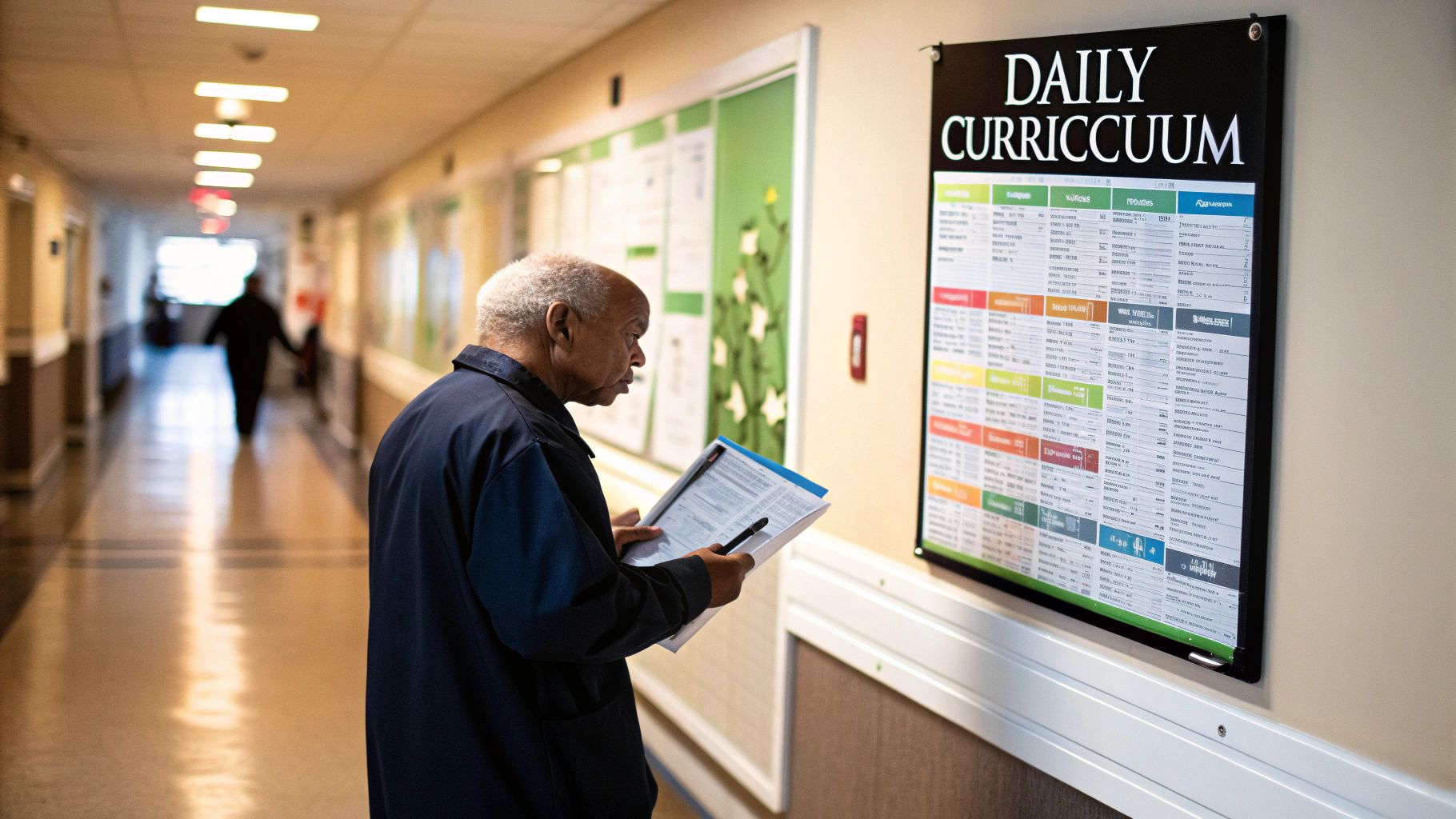
Understanding the curriculum's DNA allows you to assess whether the program’s educational philosophy aligns with your learning style. Some residents thrive in a highly structured, traditional block schedule, while others prefer a more flexible, individualized pathway. The answer to this question reveals the program's priorities and its approach to building competent, independent physicians.
How to Dig Deeper into Curriculum Structure
Go beyond the general overview provided on the program's website. Your goal during the interview is to understand the practical application of their curriculum.
Here are specific areas to explore:
- Rotation Balance: Ask about the ratio of inpatient to outpatient experiences. An internal medicine program might have a 4+1 schedule (four weeks of a core rotation followed by one week of ambulatory clinic), while another uses traditional month-long blocks. For surgical specialties, inquire about the balance between operative time and clinic responsibilities.
- Didactic Learning: How is protected academic time truly handled? Ask for a sample weekly conference schedule. Is it a series of traditional lectures, or does it include interactive formats like case-based learning, journal clubs, or resident-led morbidity and mortality (M&M) conferences?
- Skill Development: Inquire about specific training opportunities. Does the program offer dedicated simulation lab sessions for procedures? Are there structured POCUS (Point-of-Care Ultrasound) curricula with opportunities for certification?
Pro Tip: Frame your question around evolution. Ask, "What are the most recent changes you've made to the curriculum based on resident feedback, and what future changes are being considered?" This shows your interest in a dynamic, responsive training environment.
By asking detailed questions about the curriculum, you demonstrate a serious commitment to your education and gain invaluable insight into what your life as a resident in that program would actually look like. This information is critical for comparing programs and making a well-informed decision for your rank list.
2. What research opportunities are available and what support is provided?
For applicants aspiring to a career in academic medicine or aiming for a competitive fellowship, this is one of the most critical questions to ask residency programs. A program’s commitment to scholarly activity is a direct indicator of its academic rigor and its ability to prepare you for the next steps in your career. The infrastructure for research, from faculty mentorship to funding and statistical support, can vary dramatically and will define your capacity to produce meaningful work during your training.

Understanding the research landscape at a potential program helps you gauge whether your academic goals are feasible. Some programs integrate scholarly activity as a core, required component for all residents, while others offer it as an elective pathway for those with a specific interest. The answer reveals how well the program supports residents in moving beyond clinical duties to become contributors to the broader medical field.
How to Dig Deeper into Research Support
Simply knowing that "research is available" is not enough. You need to understand the practical resources and systems in place that facilitate resident-led projects from conception to publication.
Here are specific areas to explore:
- Mentorship and Guidance: Ask how residents are paired with faculty mentors. Is there a formal process or is it up to the resident to initiate contact? Inquire about the track record of these mentors in publishing with residents.
- Dedicated Time and Funding: Does the program offer protected research time or even dedicated research years? Ask if there is institutional funding available for resident projects, such as grants to cover statistical analysis or travel funds to present at national conferences.
- Infrastructure and Resources: What kind of institutional support exists? Inquire about access to statisticians, research coordinators, or IRB navigation assistance. A program with robust infrastructure significantly lowers the activation energy required to get a project off the ground. Getting involved in research as a medical student can provide a strong foundation; you can build a competitive residency application with a background in medical student research.
Pro Tip: Ask for concrete examples. Say, "Could you tell me about a few recent projects that residents have presented or published?" or "What percentage of your graduating residents who applied for fellowship matched into their top choice specialty?" This pushes for evidence of the program's success.
By asking detailed questions about research, you signal your ambition and a serious interest in an academic career. More importantly, you gather the specific information needed to determine if the program can provide the platform you need to achieve your long-term professional goals.
3. How does the program support resident wellness and work-life balance?
The demanding nature of residency training makes this one of the most vital questions to ask residency programs. Burnout is a significant and well-documented challenge in medicine, and a program’s commitment to resident wellness is not just a perk; it's a critical component of a sustainable and effective training environment. A program that actively fosters well-being creates physicians who are more resilient, engaged, and better equipped to provide high-quality patient care.

Exploring a program's approach to wellness reveals its culture and how much it values its residents as people, not just as learners and workers. To gain a deeper understanding of the challenges residents might face, it's beneficial to explore understanding the psychological impact of burnout and rebuilding resilience. The answer to this question goes beyond free lunches and yoga sessions; it speaks to the core infrastructure designed to protect and support you through the toughest years of your medical career.
How to Dig Deeper into Wellness and Work-Life Balance
Look for concrete systems and a proactive culture, not just reactive measures. Your goal is to determine if wellness is a genuine priority integrated into the program's fabric.
Here are specific areas to explore:
- Structured Initiatives: Ask about specific, tangible resources. Does the program have a dedicated wellness committee with a resident voice? Are there scheduled wellness days or retreats? Inquire about access to confidential mental health services that are easily accessible and destigmatized.
- Work-Life Integration: How does the program support residents with families or significant personal commitments? Ask about parental leave policies for both parents, the availability of backup childcare, and whether the call schedule is flexible.
- Culture of Support: Gauge the environment by asking current residents how they feel the program responds when a colleague is struggling. Is there a formal peer support or mentorship program in place? How does leadership model work-life balance? The high-stakes nature of medical training can often contribute to USMLE exam burnout, a pattern that effective wellness programs aim to counteract.
Pro Tip: When speaking with residents, ask a direct but open-ended question like, "Can you share an example of a time you felt genuinely supported by the program during a difficult period?" Their specific stories will be far more revealing than a list of official policies.
By prioritizing this question, you demonstrate maturity and a long-term perspective on your career. You are not just looking for a place to train; you are looking for a community that will support your growth and help you thrive both professionally and personally.
4. What is the case volume and patient diversity like?
The quality of your residency training is directly proportional to the quality and quantity of your clinical encounters. This question gets to the heart of the hands-on experience you will gain, exploring both the breadth (patient diversity) and depth (case volume and complexity) of a program's patient population. It’s a critical question to ask residency programs because sufficient exposure is not just about meeting graduation requirements; it’s about building the confidence and competence to practice independently after you finish training.

A program at a safety-net hospital will offer a different experience than one at a tertiary care referral center or a community hospital. Understanding this mix is crucial for aligning the program’s strengths with your career goals. Whether you want to see a high volume of "bread and butter" cases or manage rare, complex pathologies, the answer to this question will reveal if a program can provide the clinical training you need.
How to Dig Deeper into Clinical Exposure
Move beyond a simple "Do you have a diverse patient population?" and ask for specifics that illustrate the daily clinical reality for residents. Your goal is to quantify the experience.
Here are specific areas to explore:
- Case Numbers & Distribution: For procedural specialties like surgery or anesthesiology, ask graduating residents if they felt they easily met their case minimums. Inquire how high-demand or interesting cases are assigned. For internal or family medicine, ask about the typical patient census on an inpatient service.
- Patient Demographics: Probe into the socioeconomic, cultural, and linguistic diversity of the patient base. Ask, "What are the most common patient populations you serve, and what unique clinical challenges do they present?" This reveals the program's role in its community.
- Site-Specific Experience: If the program includes rotations at different hospitals (e.g., a county hospital, a VA, and a private academic center), ask how the patient population and case acuity differ at each site. This shows you how your experience will vary throughout training.
Pro Tip: Frame your question around preparation. Ask a senior resident, "Looking back, were there any specific types of cases or patient populations you wish you had more exposure to before graduating?" This can reveal potential gaps in the clinical experience.
By investigating the case volume and patient diversity, you ensure the program offers a robust and comprehensive clinical foundation. This knowledge helps you assess whether you will emerge from residency as a well-rounded physician, prepared for the challenges of your chosen specialty and ready to serve any community effectively.
5. What career support and job placement assistance is provided?
While the immediate focus of residency is training, the ultimate goal is a successful and fulfilling career. Asking about career support is one of the most critical questions to ask residency programs because it reveals their investment in your long-term future, not just your performance during training. A program that actively supports your transition into fellowship, academia, or private practice demonstrates a deep commitment to its graduates' success and recognizes that residency is a stepping stone, not the final destination.

Understanding a program's approach to career development helps you gauge the strength of its network and its ability to prepare you for the professional landscape after graduation. Some residencies are fellowship powerhouses, while others excel at placing graduates in competitive private practice jobs. The answer to this question clarifies whether the program’s resources and connections align with your specific career ambitions.
How to Dig Deeper into Career Support
Look beyond a simple "yes, we help with that." You want to understand the tangible mechanisms and track record of their career development system.
Here are specific areas to explore:
- Fellowship Placement: If you are interested in a fellowship, ask for their match statistics over the past three to five years. Inquire about the mentorship process for fellowship applications, including who helps with personal statements, interview prep, and letters of recommendation.
- Private Practice & Academic Tracks: For those considering a non-fellowship path, ask what resources are available. Does the program offer workshops on contract negotiation, billing and coding, or the business side of medicine? Do they connect residents with local physician groups or academic faculty positions?
- Alumni Network: A strong, engaged alumni network is an invaluable asset. Ask how the program facilitates connections with graduates. Are there formal mentorship programs or networking events that put current residents in touch with alumni in their desired field or location?
- Dedicated Mentorship: How are mentors assigned? Is there a formal faculty advisor system dedicated to career planning that begins early in residency, or is it an informal process left up to the resident to initiate?
Pro Tip: Ask current senior residents about their experience. Say, "For the residents who are graduating, what has the job or fellowship search process been like, and how has the program supported you through it?" This provides a real-time, unfiltered view of the support system in action.
By inquiring about career support, you demonstrate foresight and a proactive approach to your professional journey. A program with a robust, structured system for career placement is more likely to provide the guidance, connections, and skills you need to achieve your long-term goals.
6. How are residents evaluated and what feedback mechanisms exist?
The transition from medical student to resident involves a steep learning curve, and the quality of feedback you receive is paramount to your growth as a physician. A program’s evaluation system is more than just a grading rubric; it reflects its commitment to resident development, mentorship, and support. Asking this question helps you understand how the program fosters a culture of continuous improvement and ensures you are meeting critical developmental milestones.
Understanding the feedback loop is one of the most practical questions to ask residency programs because it reveals how you will be guided and supported. A strong, transparent evaluation process helps identify areas for improvement early, provides actionable advice, and empowers you to take ownership of your professional growth. Conversely, a program with vague or infrequent feedback can leave residents feeling unsupported and unsure of their progress.
How to Dig Deeper into Evaluations and Feedback
Move beyond a simple "yes, we give feedback" and probe for the specifics of the process. Your goal is to see if the system is structured, timely, and genuinely constructive.
Here are specific areas to explore:
- Frequency and Format: How often is formal feedback given? Is it at the end of each rotation, semi-annually with a program director, or a combination? Ask if feedback is delivered through a formal meeting, a written electronic evaluation, or both. For example, some programs have structured monthly one-on-one sessions with a faculty advisor.
- Types of Evaluation: Inquire about the different evaluation methods used. Do they rely solely on attending feedback, or do they incorporate a 360-degree evaluation model that includes input from peers, junior residents, nurses, and even patients? This multi-source feedback provides a more holistic view of your performance.
- Supporting Struggling Residents: How does the program identify and support residents who are not meeting milestones? Ask about the process. Is there a formal remediation plan, increased mentorship, or access to academic coaches? The answer demonstrates the program’s commitment to resident success rather than being punitive.
Pro Tip: Inquire about the resident's role in the process. Ask, "How is resident feedback on faculty and the program itself collected and used to implement change?" This shows your interest in a reciprocal, collaborative environment where everyone is accountable for improvement.
By thoroughly investigating the evaluation and feedback mechanisms, you gain insight into the program’s culture of education and support. It helps you find a place that will not only train you to be a competent physician but will also actively invest in your personal and professional development every step of the way.
7. What is the program culture and how do residents interact with each other and faculty?
While curriculum and research opportunities are tangible metrics, the program's culture is the invisible force that shapes your daily life, mental well-being, and overall satisfaction. This is one of the most critical questions to ask residency programs because a supportive, collegial environment can make the toughest rotations manageable, while a toxic one can lead to burnout. Culture dictates how residents support one another, how approachable the faculty is, and whether the program feels like a team or a collection of individuals.
Understanding the program’s culture helps you determine if you will feel a sense of belonging. The "vibe" of a residency-whether it's highly competitive, family-like, or intensely academic-directly influences your ability to learn, ask for help, and thrive under pressure. A program's culture is a reflection of its values in action, and finding a match is just as important as finding the right curriculum.
How to Dig Deeper into Program Culture
Assessing culture requires more than just asking a single question; it requires observation and targeted inquiries to understand the underlying dynamics. Your goal is to get a genuine feel for the day-to-day interactions.
Here are specific areas to explore:
- Resident Relationships: Ask residents directly, "How do you and your co-residents support each other during difficult rotations?" and "What do you do for fun together outside of the hospital?" Look for genuine camaraderie versus professional courtesy. Programs with strong peer bonds often have resident-led social committees, wellness initiatives, or informal gatherings.
- Faculty-Resident Dynamics: Inquire about the nature of faculty interaction. Is it a rigid hierarchy, or is there an open-door policy? You could ask, "Can you share an example of a time you received valuable mentorship from a faculty member outside of a formal rotation?" The answer reveals how approachable and invested the attending physicians are.
- Conflict Resolution and Support: How does the program handle resident disagreements or feedback about the curriculum? Ask, "What is the process for residents to voice concerns, and how are they addressed by leadership?" A transparent and fair process is a hallmark of a healthy culture.
Pro Tip: Pay close attention during pre-interview socials or resident-only Q&A sessions. Observe how residents interact with each other. Do they seem genuinely happy and supportive? This informal observation can be more telling than any prepared answer. For more insights on how to present yourself and assess these dynamics, check out this guide to medical residency interview preparation.
By asking about culture, you're investing in your own well-being for the next several years. A positive and supportive environment will not only make you a better physician but will also make the challenging journey of residency a more rewarding and sustainable experience.
8. What resources and technology are available for clinical care and education?
The tools at your disposal during residency shape not only your efficiency but also the very way you learn and practice medicine. This question about resources is vital because it reveals the program's investment in providing modern, effective, and supportive training. Access to advanced technology, robust electronic medical records (EMR), and comprehensive educational platforms can significantly reduce administrative burdens, enhance diagnostic accuracy, and prepare you for the realities of contemporary medical practice.
A program with up-to-date resources demonstrates a commitment to staying current and providing the best possible environment for both patient care and resident education. Conversely, outdated systems can lead to daily frustrations, inefficiencies, and a gap between your training and real-world practice. Understanding a program's technological infrastructure is crucial for gauging how well-supported you will be in your clinical and academic responsibilities.
How to Dig Deeper into Resources and Technology
Move beyond simply asking if they have an EMR. Focus on how technology is integrated into the workflow and learning process to make your life easier and your education better.
Here are specific areas to explore:
- Clinical Workflow Tools: Ask about their EMR system (e.g., Epic, Cerner) and its features. Is there remote access from home? Do they have a well-integrated mobile app for rounding? Are there efficient dictation services like Dragon or AI-powered scribes to reduce note-writing time?
- Educational Resources: Inquire about the library services and online subscriptions. Do residents get institutional access to resources like UpToDate, VisualDx, or major specialty-specific journals? Are there stipends provided for educational materials or conference travel?
- Simulation and Advanced Training: Does the program have a dedicated simulation center for procedural training? For surgical or procedure-heavy specialties, ask about access to virtual reality trainers, robotics simulators, or advanced anatomical models. This is one of the key questions to ask residency programs to assess their commitment to hands-on skill development in a safe environment.
Pro Tip: Ask current residents a practical question like, "How much of your time outside of clinical hours is spent on documentation, and what tools does the program provide to make that process more efficient?" Their answer will give you a realistic picture of the day-to-day technological support.
By investigating the available resources, you gain insight into the program’s priorities and its dedication to fostering an efficient, modern, and supportive learning environment. This knowledge helps you envision your daily workflow and determine if the program is equipped to prepare you for the future of medicine.
Residency Program Questions Comparison
| Aspect | Training Curriculum ⭐🔄📊💡 | Research Opportunities ⭐🔄📊💡 | Resident Wellness ⭐🔄⚡💡 | Case Volume & Diversity ⭐📊💡 | Career Support ⭐⚡📊💡 | Evaluation & Feedback ⭐🔄💡 | Program Culture ⭐🔄💡 | Resources & Technology ⭐⚡📊💡 |
|---|---|---|---|---|---|---|---|---|
| Implementation Complexity (🔄) | Moderate; involves structured rotations & sessions | High; requires dedicated time, mentorship & funding | Moderate; wellness programs vary in depth | Moderate; tracking case data & exposure | Moderate; career services and networking required | Moderate; needs structured feedback systems | Low to moderate; culture influenced by leadership | Moderate to high; investment in tech & training |
| Resource Requirements (⚡) | Clinical and educational staff, facilities | Research faculty, funding, lab space | Counseling services, wellness coordinators | Diverse patient population, multi-site facilities | Career advisors, alumni networks, event resources | Faculty time for evaluations, data systems | Investment in community-building activities | Advanced tech systems, simulation centers |
| Expected Outcomes (📊) | Competent, well-rounded clinicians | Scholarly activity & academic career preparation | Improved resident well-being, reduced burnout | Adequate clinical competence, board eligibility | Successful job/fellowship placement | Continuous resident growth, early issue identification | Supportive, collaborative learning environment | Enhanced clinical care and education efficiency |
| Ideal Use Cases (💡) | Applicants valuing structured learning pathways | Those pursuing academic/research-focused careers | Residents prioritizing mental health and balance | Candidates wanting broad, diverse clinical exposure | Residents aiming for clear career progression | Trainees needing frequent feedback and growth plans | Applicants valuing strong support and collegiality | Programs emphasizing modern medical practice |
| Key Advantages (⭐) | Clear progression, wide clinical exposure | Strong mentorship, academic prestige | Burnout prevention, wellness culture | Exposure variety, meets certification requirements | Networking, career guidance, alumni engagement | Promotes professionalism, proactive remediation | Enhances satisfaction, supports learning | Prepares for future practice, improves learning speed |
Crafting Your Rank List with Confidence
The residency interview trail is an exhaustive yet illuminating journey. After countless virtual meetings, hospital tours, and conversations with faculty and current residents, you are now armed with a wealth of information. The exhaustive list of questions to ask residency programs provided in this guide was not just about ticking boxes; it was about gathering the crucial data points needed to make one of the most significant decisions of your professional life. Now, the final and most critical phase begins: synthesizing this information to confidently build your rank order list.
This process is far more than just a gut feeling. It’s about methodically cross-referencing the answers you received against your personal and professional priorities. The goal is to move beyond the superficial allure of a program's reputation and delve into the daily realities of training there.
Synthesizing the Data: From Questions to a Clear Choice
Think back to the core themes we explored. Your task is to transform abstract interview notes into a concrete, comparative analysis. Create a spreadsheet or a decision matrix. List your top programs across the top and the key question categories down the side. This structured approach prevents you from forgetting critical details and helps mitigate recency bias, where the last program you interviewed with feels like the best one.
Curriculum and Training Structure: Did one program’s educational philosophy resonate more strongly? Perhaps a program with a heavy emphasis on early autonomy feels invigorating, while another’s structured, didactic-heavy approach provides the foundation you crave. Go back to your notes. A vague "good curriculum" isn't enough. Note specific details: "X+Y schedule allows for dedicated study time," or "Integrated longitudinal clinic from PGY-1 offers better continuity of care."
Culture and Wellness: This is often the deciding factor. Culture is an intangible feeling backed by tangible evidence. Did residents seem genuinely happy and collaborative? Were wellness initiatives practical and utilized, or just a talking point? Consider the program's response to your questions about resident support. A program that openly discusses challenges and has established systems for feedback and mental health support is often more genuinely invested in its trainees than one that offers superficial perks.
Career Goals and Mentorship: Your residency is the launchpad for your career. Re-evaluate the answers regarding research support, career development resources, and alumni networks. If your goal is a competitive fellowship, a program with a strong track record of fellowship matches and dedicated research time is non-negotiable. If you envision a career in private practice, a program with robust community rotations and business-of-medicine didactics might be the superior choice.
Key Insight: The "best" program does not exist in a vacuum. The best program is the one that offers the ideal environment for you to thrive, learn, and grow into the physician you aspire to be. Your rank list is a declaration of your unique needs and goals.
Trusting Your Informed Intuition
After methodically analyzing the data, allow your intuition to play a role. Where did you feel the most at ease? Which group of residents could you picture yourself working with on a grueling 30-hour call? Often, your gut feeling is your subconscious processing thousands of small data points, from body language to the energy of a room. When your data-driven analysis aligns with your personal feeling of "fit," you have found a powerful combination.
By leveraging this comprehensive list of questions to ask residency programs, you have done the hard work. You have moved beyond the brochure and engaged in a deep, investigative process. This diligence empowers you to approach Match Day not with apprehension, but with the quiet confidence that comes from making a well-informed, strategic, and deeply personal decision. You have laid the groundwork for a successful and fulfilling start to your medical career.
Navigating the complexities of the residency match process requires more than just a great application; it demands strategic preparation. At Ace Med Boards, our expert tutors and consultants specialize in providing personalized residency admissions consulting, from interview coaching to rank list strategy. We help you articulate your strengths and find the program that perfectly aligns with your career aspirations. Ace Med Boards
