When you’re faced with a thyroid panel, the smartest move is to look at TSH first. It’s your primary gatekeeper for thyroid disorders. With a normal range of 0.4–4.0 mIU/L, most decisions start here.
Quick Thyroid Test Patterns
A streamlined hierarchy will help you tell overt from subclinical cases in seconds.
- TSH Remains Your First-Line Marker (0.4–4.0 mIU/L)
- Free T4 Comes Next To Sidestep Binding Protein Fluctuations
- Total T4 Steps In When You Suspect Protein-Binding Anomalies
- T3/Reverse T3 Use In T4-Normal Hyperthyroidism Or Amiodarone Therapy
- Thyroid Antibodies Confirm An Autoimmune Process
Once you’ve gathered those values, patterns emerge quickly. High TSH with low free T4 points to overt hypothyroidism, while a normal free T4 with elevated TSH suggests a subclinical picture. Low TSH alongside a high free T4? Think hyperthyroidism.
Laboratory Interpretation Summary Table
Here’s a side-by-side comparison of the classic TSH/free T4 combinations and their most likely diagnoses. Use this as a rapid-reference tool during rounds or exam prep.
| Pattern | TSH | Free T4 | Diagnosis |
|---|---|---|---|
| High TSH + Low Free T4 | ↑ | ↓ | Overt Hypothyroidism |
| High TSH + Normal Free T4 | ↑ | ↔ | Subclinical Hypothyroidism |
| Low TSH + High Free T4 | ↓ | ↑ | Hyperthyroidism |
That quick snapshot should cut down your interpretation time. Keep it handy when you need to triage lab results under pressure.
It underscores the tight relationship between TSH and free T4, reinforcing the sequence above. For a deeper dive into pattern recognition, check out this detailed review on thyroid dynamics from the Journal of Thyroid Research.
Key Insights
- Always Start With TSH, Then Confirm With Free T4 And Antibodies.
- Remember That Total T4 Levels Fluctuate When Binding Proteins Shift.
- Reserve T3 Measurements For Discordant Cases Or Specific Therapies.
- Correlate Every Lab Value With The Patient’s Symptoms And History.
Key Takeaway: Labs guide you, but the clinical picture seals the diagnosis.
By keeping these pointers in mind, you’ll interpret thyroid panels like a pro—whether you’re on the wards or tackling exam questions.
Understanding Key Thyroid Tests
Thyroid panels give us a snapshot of gland function by measuring key hormones and antibodies. Interpreting these values correctly is crucial for distinguishing between hypo- and hyperthyroid states.
TSH remains our most sensitive marker when teasing out primary gland disorders from central causes. With a normal range of 0.4–4.0 mIU/L, values above that suggest hypothyroidism, while values below point toward hyperthyroidism. In one large series, 11% of TSH assays fell outside the reference range—64.6% indicated underactive thyroid and 26.4% pointed to overactivity. Learn more on PMC.
In the U.S., about $1.6 billion is spent on thyroid testing each year, and 75% of that volume is TSH alone. That frequency underlines why it’s wise to retest borderline results before making treatment decisions. Free T4 sidesteps protein-binding issues to show active hormone levels, whereas total T4 can reveal shifts in binding proteins.
T3 and reverse T3 assays play more specialized roles. T3 helps clarify T4-normal hyperthyroidism and assesses peripheral conversion, while reverse T3 spikes in critical illness, flagging euthyroid sick syndrome.
• TSH – Pituitary feedback and primary gland function
• Free T4 – Unbound, biologically active hormone
• Total T4 – Reveals binding protein interference
• T3 – Gauges peripheral conversion and overt hyperthyroidism
• Reverse T3 – Signals non-thyroidal illness or acute stress
• Anti-TPO & Anti-Tg – Confirm autoimmune involvement
Lab Methodologies Explained
Most TSH and free T4 values come from immunoassays. Competitive assays for free T4 accurately isolate the unbound fraction, but preanalytical factors can still trip us up:
- Temperature control during transport
- Timing relative to medication doses
- Hemolysis, lipemia or clotting artifacts
- High-dose biotin interference
For a deeper dive into how these tests tie into core endocrine principles, check out our detailed Endocrine System Study Guide.
Reverse T3 And Antibody Insights
Reverse T3 often climbs in critical illness, reminding us to hold off on unnecessary thyroid hormone replacement. Antibody assays, like anti-TPO and anti-Tg, chart autoimmune activity and help predict when to start treatment. Higher titers generally correlate with more active disease.
Key Insight: High anti-TPO levels paired with an elevated TSH almost always indicate Hashimoto’s thyroiditis.
| Antibody | Positive Threshold | Disease Association |
|---|---|---|
| Anti-TPO | >35 IU/mL | Hashimoto’s disease |
| Anti-Tg | >40 IU/mL | Hashimoto’s disease |
Assay Interference Tips
Unexpected lab values warrant a second look—often the culprit is assay interference:
- Heterophile or cross-reactive antibodies
- Rheumatoid factor
- Macro-TSH complexes
- Variability in assay reagents
Whenever results don’t fit the clinical picture, repeat testing using a different method. And don’t forget to ask patients to pause high-dose biotin 48 hours before their blood draw.
Clinical Correlation And Pitfalls
Lab numbers don’t stand alone. Always weave in history, physical findings and imaging before diagnosing or adjusting therapy. Trends matter more than isolated readings—especially when TSH hovers near the cutoff.
- Retest borderline TSH after 6–8 weeks before making changes.
- Central hypothyroidism usually shows low or “inappropriately normal” TSH alongside low T4.
- Consider TRH stimulation testing or pituitary imaging for equivocal cases.
- Adjust reference ranges for pregnancy (first-trimester TSH ~0.1 mIU/L) and the elderly (upper limit near 6 mIU/L).
Master these nuances, and you’ll navigate thyroid test interpretation with confidence.
Practical Algorithm For Test Interpretation
When TSH drifts outside its normal range, the entire evaluation pivots. A high TSH points you toward hypothyroid patterns, while a low TSH steers you to hyperthyroid possibilities. From there, free T4 becomes your next checkpoint—confirming whether the gland is really over- or under-producing.
In the real world, lab numbers don’t exist in isolation. Always tie them back to medications, supplements and acute illnesses. For instance, biotin can wreck immunoassay results, and a serious infection might push reverse T3 sky-high without true hyperthyroidism. Let’s walk through the pathways you’ll encounter on rounds or exams, complete with examples and a clear decision tree.
- Evaluate Free T4 whenever TSH is above 4.0 mIU/L or below 0.4 mIU/L to nail down unbound hormone activity.
- Compare Total T4 when you suspect alterations in binding proteins (think pregnancy or nephrotic syndrome).
- Measure T3 and reverse T3 in discordant or critical-illness cases—especially if free T4 and TSH don’t tell the full story.
- Order antibody panels only when your TSH–free T4 pattern hints at autoimmune thyroid disease.
These steps keep TSH front and center, while adapting to assay quirks and complex presentations. Below, each section breaks down how to interpret primary, central and non-thyroidal patterns with practical pointers.
Key Point: Use TSH as your launchpad, then confirm with free T4 before committing to a diagnosis.
Assessing TSH Results
TSH sits at the top of your flowchart because it mirrors pituitary feedback.
A value above 4.0 mIU/L usually means primary hypothyroidism.
By contrast, a TSH below 0.4 mIU/L raises concern for hyperthyroidism or central suppression. Always match these lab results with symptoms—fatigue, weight gain or palpitations can tip you off.
When you see high TSH but normal free T4, you’re in subclinical territory.
In practice, you’d monitor those levels over 6–8 weeks before deciding on levothyroxine or further workup.
This pause prevents unnecessary treatment.
Evaluating Free T4 And Binding Issues
Free T4 cuts through binding-protein noise, offering a clear view of active hormone levels.
But total T4 still has its use in settings where binding proteins fluctuate—like estrogen therapy or heavy proteinuria.
If total T4 is off but free T4 holds steady, trust the free fraction.
| Pattern | TSH | Free T4 |
|---|---|---|
| Primary Hypothyroidism | ↑ | ↓ |
| Subclinical Hypothyroidism | ↑ | ↔︎ |
| Central Hypothyroidism | ↓ or normal | ↓ |
Compare your thyroid labs with albumin and TBG when you suspect binding disorders.
Labs often include total T3 alongside total T4—spotting an odd total T4 frees you from a misdiagnosis.
Integrating T3 And Reverse T3
You’ll turn to T3 measurement when free T4 is high but TSH is only mildly suppressed, or in patients on amiodarone.
Reverse T3 spikes in non-thyroidal illness and severe stress.
A pattern of low active hormones and high reverse T3 screams euthyroid sick syndrome.
Recognizing this saves patients from unnecessary thyroid treatment.
If assays conflict or patient factors muddy the waters, loop back to your TSH–free T4 framework.
Always keep assay interference and biotin in mind.
For suspected central dysfunction, don’t hesitate to pull in endocrinology or consider pituitary imaging.
Ordering Antibody Tests For Clarity
Autoimmune tests belong when your TSH–free T4 pattern suggests it.
An elevated TSH with low free T4 plus positive anti-TPO seals a Hashimoto’s diagnosis.
High anti-TSHR in a hyperthyroid patient confirms Graves’ disease.
Reflex antibodies can save time and reduce costs—just don’t order them blindly.
Let clinical clues (rapid gland enlargement, family history) guide your decision.
Below is the vertical decision tree from TSH to free T4 and finally antibodies.
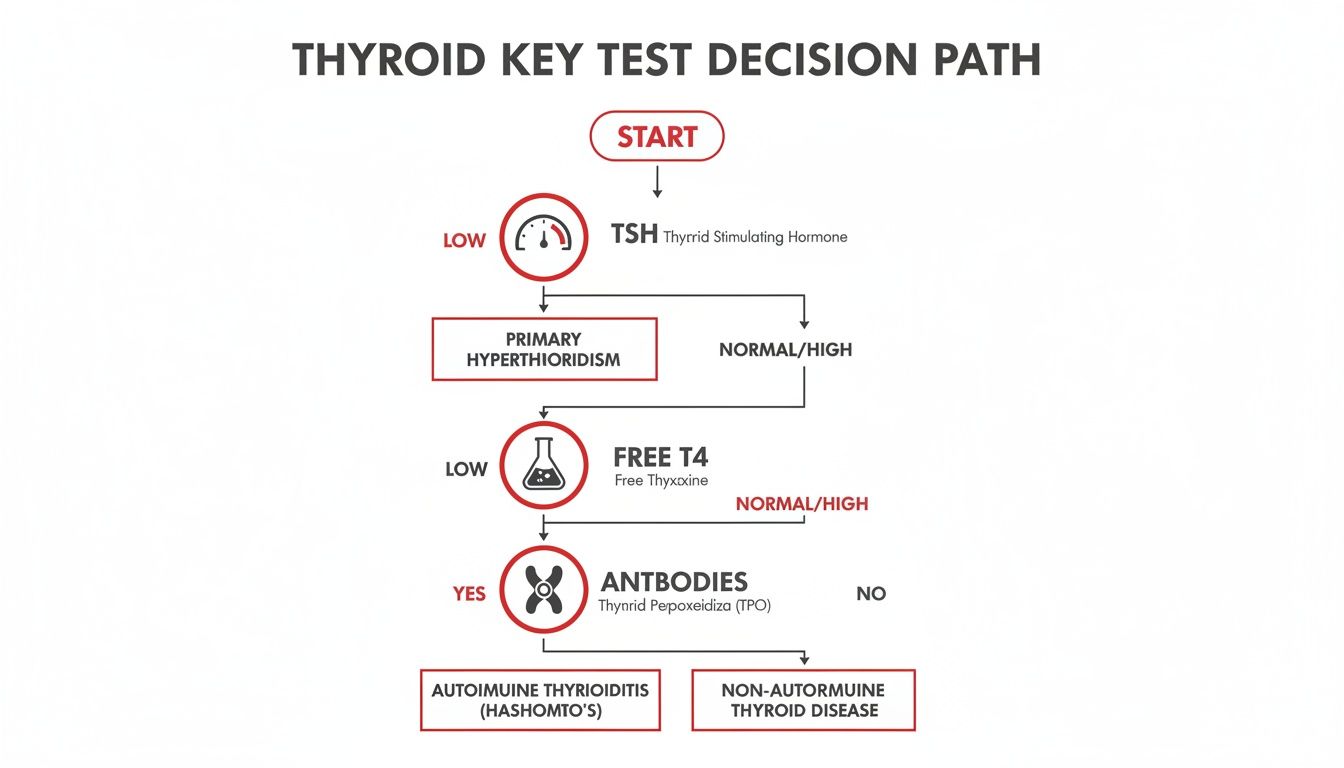
This diagram shows how an out-of-range TSH triggers free T4 measurement, and how antibody testing slots in when earlier results remain inconclusive.
Handling Complex Clinical Scenarios
Critical illness can flip your labs—think low T3 with high reverse T3 in euthyroid sick syndrome.
Central hypothyroidism shows a low-normal TSH with low free T4.
Drugs like amiodarone or high-dose steroids also disturb thyroid assays and warrant a deeper dive.
Tailor your interpretation to each patient:
- Review supplements (biotin, iodine) and prescription meds.
- Align lab changes with clinical signs before labeling dysfunction.
- Repeat borderline results after 6–8 weeks to avoid hasty interventions.
- Adjust reference ranges for age, pregnancy trimesters or other physiologic states.
This dynamic roadmap equips you to tackle straightforward and tricky thyroid panels alike. Next, we’ll apply these principles in real patient cases to sharpen your clinical reasoning and prep you for exam scenarios.
You might also find our approach to differential diagnosis useful whenever labs remain unclear: What Is Differential Diagnosis.
Role Of Antibodies And Imaging In Diagnosis
Combining antibody assays with imaging deepens diagnostic accuracy in thyroid disorders. Rather than relying on a single test, this dual approach confirms autoimmune involvement and often spares patients from unnecessary biopsies.
- Anti-TPO and Anti-Tg levels to spot Hashimoto’s or Graves’
- Neck ultrasound for nodule vs diffuse disease patterns
- Radioiodine uptake scans to pinpoint hyperactive tissue
- Antibody titers to inform management of subclinical cases
Antibody tests act as a bridge between raw lab numbers and the clinical picture. When you see a high TSH paired with positive Anti-TPO or Anti-Tg, autoimmune hypothyroidism slides to the top of your differential.
A combination of elevated antibodies, high TSH and low T4 crops up in 7.5% of patients worldwide—and it’s roughly four times more common in women. For subclinical hypothyroidism (TSH 4.5–10 mIU/L, normal T4), the presence of antibodies often nudges us toward early treatment rather than watchful waiting.
Read the full research about Hashimoto’s prevalence on Frontiersin: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.1020709/full

Deciding which assays and scans to order always circles back to patient history, physical exam and lab trends. These clues guide both the sequence and nature of testing.
Antibody Testing For Autoimmune Thyroid Disease
Tracking antibody titers over time offers real insight into disease activity. A sharp rise in Anti-TPO suggests active Hashimoto’s, while an uptick in Anti-Tg adds another layer of confidence.
Most clinicians repeat antibody panels every 6–12 months in patients with borderline lab values. It’s a simple way to catch a shift from subclinical to overt disease before symptoms emerge.
When Should You Order Antibodies?
- TSH above 4.5 mIU/L with normal free T4
- Clinical suspicion of autoimmune thyroiditis based on exam or history
Skipping antibody tests without a clear lab or exam trigger can lead to overtesting—and patient anxiety. Positive results in a borderline case often tip the balance toward early intervention, cutting overt hypothyroidism by around 20% at follow-up.
Before moving on to imaging, lock in the serologic findings against your clinical suspicion.
Table: Antibody and Ultrasound Correlation
| Antibody Result | Ultrasound Pattern | Clinical Takeaway |
|---|---|---|
| High Anti-TPO | Diffuse hypoechoic gland | Confirms Hashimoto’s |
| Positive Anti-Tg | Heterogeneous texture | Supports autoimmune risk |
When serology and ultrasound tell the same story, you can proceed with confidence. Any conflicting clues should prompt a biopsy discussion or an endocrinology referral.
Imaging Modalities In Thyroid Evaluation
Ultrasound excels at distinguishing nodular disease from diffuse thyroiditis. It reveals echogenicity changes and vascular patterns that hint at underlying inflammation or neoplasm.
If lab and ultrasound results don’t align, adding a radioiodine uptake scan boosts diagnostic yield by roughly 20%. Functional imaging shows exactly which tissues are guzzling iodine—and who might benefit from radioiodine therapy.
Reserve CT or MRI for goiters with retrosternal extension or suspected invasive behavior. In most cases, the combination of ultrasound plus uptake gives all the clues you need.
Integrating Lab And Imaging Findings
Bringing together serology, ultrasound and functional scans turns a jumble of numbers into a clear roadmap. For example, a diffuse, hypoechoic gland on ultrasound paired with positive Anti-TPO seals the diagnosis of Hashimoto’s without needing a biopsy.
On the flip side, nodules with negative antibodies and low uptake scans almost always point to benign colloid nodules. If anything still feels off, fine-needle aspiration under ultrasound guidance is your next best move.
Here’s how I piece it all together:
- Review TSH and free T4 for thyroid status
- Layer in Anti-TPO / Anti-Tg titers for autoimmunity clues
- Use ultrasound to map anatomy and spot nodules
- Add uptake scans if function needs clarification
- Synthesize every result before finalizing treatment
This structured approach builds confidence—and it often saves patients from extra tests and delays. Always keep non-thyroidal illness and assay interference on your radar.
Key Points To Remember
Key Takeaway: Antibodies unmask autoimmune activity, ultrasound outlines structure, and uptake scans confirm function. Integrate all three before jumping to biopsy or treatment.
- Recheck antibody titers every 6–12 months in borderline cases
- Use imaging selectively to resolve lab or clinical discrepancies
- Tie every finding back to symptoms and exam for precise decisions
In the end, matching lab and imaging results to the patient’s story is what drives accurate, confident thyroid care.
Worked Examples And Case Studies
Sometimes your clinical instincts and lab numbers don’t line up. Working through real-life scenarios helps you see exactly how history, labs, imaging and symptoms converge. Below, each example traces a patient from presentation to final interpretation using our TSH–Free T4 algorithm.
You’ll notice the subtle decision points—what to check next, when to hold off, and how to avoid common traps. Dive in and let these cases sharpen your diagnostic radar.
Case Study: Primary Hypothyroidism
A 45-year-old woman arrives complaining of fatigue, weight gain and dry skin. Her labs show TSH 8.2 mIU/L with a Free T4 of 0.6 ng/dL (below normal). Ultrasound reveals a diffusely heterogeneous gland—no suspicious nodules.
Here’s how the picture falls into place:
- Elevated TSH reflects pituitary feedback trying to kickstart hormone production
- Low Free T4 confirms the thyroid isn’t keeping up
- Anti-TPO and Anti-Tg levels at 300 IU/mL establish Hashimoto’s thyroiditis
Catching it early in subacute phases can stop progression toward myxedema.
Starting levothyroxine and repeating labs every 6–8 weeks usually brings levels back to normal without confusion.
Case Study: Graves Disease
Our next patient is a 30-year-old man with palpitations, tremor and heat intolerance. His TSH is 0.02 mIU/L while Free T4 hits 3.2 ng/dL. A radioiodine uptake scan lights up at 65%, pointing away from thyroiditis.
Key findings:
- Suppressed TSH and high Free T4 clinch hyperthyroidism
- Diffuse uptake confirms Graves disease rather than a destructive thyroiditis
- An Anti-TSHR titer of 45 IU/L seals the diagnosis
Graves often brings eye signs or pretibial changes—keep an eye out.
Beta blockers for symptom relief and antithyroid drugs to curb hormone output let labs and clinical status sync up neatly.
Case Study: Subclinical Abnormalities
A 55-year-old gentleman has mild fatigue but no overt hypothyroid stigmata. His TSH is 5.1 mIU/L while Free T4 holds steady at 1.2 ng/dL. Negative antibodies and a clean ultrasound rule out structural disease.
When TSH creeps above normal but Free T4 remains normal, you’re in subclinical territory:
| Pattern | TSH Level | Free T4 Level | Next Step |
|---|---|---|---|
| Mild TSH Elevation | 4.5–10 | Normal | Observe and repeat labs |
| TSH Above 10 | >10 | Normal/Low | Consider levothyroxine |
| Persistent Symptoms | Any TSH | Any | Evaluate clinical impact first |
Monitoring every 3 months and reserving treatment for TSH > 10 mIU/L or worsening symptoms prevents unnecessary therapy.
Case Study: Biotin Interference
A 28-year-old who takes 5 mg daily biotin shows TSH 0.1 mIU/L and Free T4 4.5 ng/dL. Clinically, he feels fine. A quick supplement check explains the bizarre labs.
Biotin can skew immunoassays—falsely low TSH and falsely high Free T4. The fix is simple:
- Ask patients to stop biotin 48 hours before sampling
- Repeat the panel once the supplement washes out
Sure enough, follow-up labs land in normal range and hyperthyroidism is ruled out.
Key Lessons And Pitfalls
Real patients teach more than charts ever will. Patterns that look textbook can derail if you forget:
- Non-thyroidal illness (and reverse T3) can mimic dysfunction
- Supplements or heterophile antibodies may distort results
- Borderline TSH without matching symptoms rarely demands treatment
Regular case reviews build the confidence to call it right every time.
Next Steps In Practice
Whenever you see an odd thyroid panel, start by mapping TSH and Free T4 before ordering extras. Lean on these case scenarios as your mental guidebook. If you need structured support, check out Ace Med Boards for one-on-one coaching and tailored case reviews.
- Expert tutors reinforce decision-making under exam pressure
- Free consultations identify your high-yield weak spots
- Personalized cases bridge the gap between theory and real patients
Final Takeaways
- TSH Always Leads: It’s your first clue
- Free T4 Confirms: Assess active hormone levels
- Antibodies & Imaging Refine: Lock in the specific diagnosis
- Repeat Borderline: Don’t treat in a vacuum—watch, wait, then act
Apply this stepwise approach, trust the algorithm, and you’ll read thyroid panels like a seasoned clinician. Keep practicing, stay curious, and let real-world examples guide your next interpretation. Cheers!
Exam Focused Tips And Common Pitfalls
Nailing thyroid test interpretation can be the difference between a confident answer and second-guessing yourself on exam day. These pointers blend memory shortcuts with real-world traps you’ll encounter in board-style vignettes.
A solid strategy balances thresholds, lab patterns, and clinical context. You’ll find acronyms to anchor your thought process, highlighted pitfalls, and study habits that I’ve honed through personal experience.
High Yield Memory Tricks
Try “T-FAB” as your first anchor:
- T = TSH for the initial screening step
- F = Free T4 to confirm biologic activity
- A = Autoantibodies to catch autoimmune causes
- B = Binding protein shifts shown by total T4
That sequence takes seconds to run in your mind.
Follow up with “SHiFT” for hyperthyroidism:
- S = Suppressed TSH
- Hi = High free T4
- F = Follow-up uptake scan when uptake patterns matter
- T = T3 measurement if numbers don’t add up
These hooks speed recall under time pressure.
Pitfalls To Avoid
Critically ill patients often display euthyroid sick syndrome. You’ll see low T3 paired with elevated reverse T3. Treating this biochemistry in isolation is a classic exam trap.
When results clash with the clinical picture, suspect assay interference. Heterophile antibodies, rheumatoid factor, or high-dose biotin can skew immunoassays. Always review supplements if labs look off.
Relying on total hormone levels can mislead you. Pregnancy, oral estrogens, and nephrotic syndrome alter binding proteins—yet free T4 remains the real indicator of thyroid function.
Key Insight
Reference ranges aren’t one-size-fits-all. An elderly patient’s upper TSH limit may be 6.0 mIU/L, while first-trimester targets hover around 0.1–2.5 mIU/L.
| Common Mistake | Lab Clue | Correct Approach |
|---|---|---|
| Treating euthyroid sick | ↑ reverse T3, ↓ T3 | Hold therapy; recheck after recovery |
| Ignoring biotin interference | Low TSH, high free T4 | Repeat labs after 48-hour biotin washout |
| Relying on total T4 alone | Shifts in TBG | Always interpret free T4 |
Personal Exam Tips
I save time and dollars by ordering TSH with reflex free T4, not shotgun hormone panels. This habit embeds the algorithm and cuts down on red herrings.
Match lab data to the vignette. Weight gain plus bradycardia with high TSH and low free T4? Primary hypothyroidism. Don’t let distractors throw you off.
Bookmark updates from the American Thyroid Association and major reagent manufacturers. Staying current means you won’t trip over a new assay method or reference-range tweak.
Check out our guide on effective clinical decision making with this internal resource to boost your reasoning skills: learn more about clinical reasoning
Rotate through question banks that feature thyroid sections. Aim for 80% accuracy on mixed endocrine quizzes before you call yourself exam-ready.
Remember
A clear clinical story plus two key labs beats memorizing endless hormone values. Patterns always outscore raw numbers.
Avoid Overreliance On Single Tests
One lab rarely tells the whole story. An isolated low TSH in an asymptomatic patient often flags an artifact. Always confirm with history and free T4.
Use these quick checks:
- Cross-check TSH and free T4 within 24–48 hours
- If results clash, rerun on a different assay platform
- Screen for biotin, heparin, or antibody interference
Refine Chart Reviews
Fast, focused note-taking is your exam ally. Jot down vital signs—weight changes, heart rate—and sketch a two-column table: clinical findings on one side, labs on the other.
For example:
- Weight gain + bradycardia = hypothyroid pattern
- Weight loss + tremor = hyperthyroid signs
- Elevated TSH alone = subclinical hypothyroidism
Practicing this in under 10 seconds builds muscle memory.
Stay Updated With Guidelines
Exam questions often reference the latest targets and assay methods. Bookmark the American Thyroid Association’s guidelines and key lab-manufacturer bulletins. Focus on:
- First-trimester TSH: 0.1–2.5 mIU/L
- Upper TSH limit in elderly: ~6.0 mIU/L
- Role of reverse T3 in non-thyroidal illness
Blend question banks, flashcard drills, and case write-ups into your daily routine. Before test day, explain thyroid patterns aloud to a study partner—nothing cements learning like teaching.
Final Tip
Read each vignette carefully. Plot TSH and free T4 first, then layer in history and demographics for the winning answer.
Don’t forget medication effects. Amiodarone, high-dose steroids, lithium—these commonly nudge thyroid labs. Create a quick chart of 5 drugs and their typical lab shifts for instant recall.
Frequently Asked Questions
Best Initial Test For Suspected Thyroid Dysfunction
When a patient presents with fatigue, cold intolerance and weight gain, I always check TSH first. It remains the most sensitive marker of the pituitary-thyroid feedback loop. This single test flags primary and central disorders at once.
• Order TSH initially.
• If it’s outside the normal range, follow up with free T4.
Non-Thyroidal Illness Effects
In acute illness you’ll often see low T3, high reverse T3 and erratic free T4. Sepsis, trauma or systemic inflammation shifts peripheral conversion and protein binding. Ignoring this context can lead to false positives.
• Note any recent stressor or hospitalization.
• Consider reverse T3 in critically ill patients.
When To Add Antibody Tests
I request anti-TPO and anti-Tg assays when TSH and free T4 hint at autoimmune thyroiditis or subclinical hypothyroidism. Finding positive titers in borderline cases often pushes me toward earlier intervention.
• Borderline labs + compatible symptoms → check antibodies.
• Known immune disorders? Test at the outset.
Managing Subclinical Cases
If TSH sits between 4.5 and 10 mIU/L with a normal free T4, I repeat labs in 6–8 weeks and watch for evolving symptoms. Treatment usually starts once TSH exceeds 10 mIU/L or the patient reports clear clinical changes.
Expert Insights
Logging every abnormal thyroid panel improves pattern recognition and sharpens your interpretation skills.
• Quiz yourself with actual patient scenarios.
• Keep a running notebook of recurring lab quirks.
Quick Tips
Never rely on one discordant lab result. Select a few targeted tests to confirm your suspicion and reduce unnecessary costs.
• Prioritize history and exam over broad panels.
• Use clinical context to guide your lab selection.
Adjusting Reference Ranges
Age, pregnancy and assay methods shift TSH norms. Always tailor your thresholds.
• Apply age-specific cutoffs, especially in older adults.
• In pregnancy, follow trimester-specific TSH targets.
Ready to refine your interpretation skills? Join Ace Med Boards and schedule your free consultation: Ace Med Boards
