Let's be blunt: the single most effective thing you can do to prepare for the USMLE Step 2 CK is to grind through practice questions. With Step 1 now pass/fail, your Step 2 CK score has become a massive data point for residency applications. A question-centric study plan isn't just a good idea—it's absolutely essential.
Why Step 2 CK Questions Are Your Most Critical Prep Tool
Since Step 1 went pass/fail, your Step 2 CK score is no longer just another exam. It's one of the most critical numerical filters program directors use to evaluate your clinical reasoning and overall readiness for residency. That's a huge shift.
This reality completely changes how you need to prepare. Rote memorization of facts, while still part of the game, just won't cut it. The exam is built to test how you apply knowledge in messy, real-world clinical scenarios, almost always asking for the "next best step" in managing a patient.
Moving Beyond Memorization
At its core, Step 2 CK is all about the clinical vignette. You get a short patient story crammed with history, physical exam findings, and lab results, and your job is to dissect it, build a differential, and make a solid clinical decision under intense time pressure. This is a skill you can only build through repetition and deliberate practice with high-quality sample questions.
When you anchor your study time in practice questions, you're actively engaging with the material in the exact format you'll face on test day. This isn't passive learning; it's active training.
- You start seeing the patterns. After a while, you begin to recognize the classic illness scripts and high-yield presentations the NBME loves to test.
- You're forced to apply knowledge. It's one thing to know a fact; it's another to understand how that fact actually changes a clinical decision.
- You build serious stamina. Plowing through timed question blocks builds the mental endurance required for a grueling nine-hour exam.
At Ace Med Boards, our entire tutoring philosophy is built around this question-based approach. We’ve seen it time and time again: students who actively deconstruct thousands of questions consistently blow past those who just re-read textbooks or passively watch videos.
A Foundation Built on Practice
Your clerkships give you the raw clinical exposure, but practice questions are what translate that experience into a top-tier score. Every specialty, from Internal Medicine to Surgery, has its own unique flavor and common traps. Chewing through a massive volume of questions is the only way to ensure you've covered the sheer breadth of that content. For instance, knowing how to properly integrate a tool like UWorld for Step 2 can make or break your study plan.
Ultimately, a strong performance on Step 2 CK sends a clear signal to residency programs: this applicant has the clinical acumen to hit the ground running on day one. This guide will give you the framework to master those sample questions, turning your prep from a passive review into an active, score-boosting machine.
How to Break Down a High-Yield Clinical Vignette
Let's move from theory to practice. The fastest way to boost your score is to get your hands dirty dissecting high-quality USMLE Step 2 CK sample questions until the process is automatic.
We're going to walk through a classic internal medicine vignette, showing you exactly how a top-scoring student thinks, acts, and decides under pressure.
The Clinical Scenario
A 68-year-old male with a history of hypertension and hyperlipidemia presents to the emergency department with 2 hours of substernal chest pain. He describes the pain as a "crushing" sensation that radiates to his left arm. He is diaphoretic and appears anxious. An EKG shows ST-segment elevations in leads II, III, and aVF. His blood pressure is 88/60 mmHg, and his heart rate is 110/min. Physical examination reveals clear lung sounds bilaterally.
What is the most appropriate next step in management?
A) Administer intravenous fluids
B) Administer nitroglycerin
C) Administer metoprolol
D) Perform urgent percutaneous coronary intervention (PCI)
E) Obtain a chest X-ray
Pinpointing the Crucial Clues
First thing's first: let's pull out the pieces that actually matter. This isn't just a random list of facts; it's a story, and every clue is pointing you toward the diagnosis.
- Patient Demographics and History: 68-year-old male with hypertension and hyperlipidemia. Right away, you should be thinking about coronary artery disease. These are textbook risk factors.
- Chief Complaint: "Crushing" substernal chest pain radiating to the left arm. This is the classic, can't-miss-it presentation for an acute myocardial infarction (MI).
- EKG Findings: ST-segment elevations in leads II, III, and aVF. This is huge. It doesn't just tell you he's having an MI; it pinpoints the location to the inferior wall of the heart.
- Vital Signs: Hypotension (88/60 mmHg) and tachycardia (110/min). This is a red flag. The patient is unstable.
- Physical Exam: Clear lungs. This is a critical negative finding. It helps you rule out things like acute heart failure, which would likely cause pulmonary edema (crackles in the lungs).
When you put it all together, what do you have? An older man with cardiac risk factors who is having a full-blown inferior wall ST-elevation myocardial infarction (STEMI) and is now in cardiogenic shock.
This combination of an inferior STEMI plus hypotension is a high-yield pattern that should scream one thing in your brain: right ventricular infarction.
Analyzing the Answer Choices
Okay, now that we have a working diagnosis, let's attack the answer choices. The question asks for the "most appropriate next step," which means we have to think about priorities. What saves this patient's life right now?
A) Administer intravenous fluids: Patients with an RV infarct are incredibly dependent on preload to keep blood pumping. Their right ventricle is stunned and can't contract well, so they need all the volume they can get to push blood forward. Giving IV fluids would increase that preload and almost certainly help his blood pressure. This is a very strong contender.
B) Administer nitroglycerin: Nitroglycerin is a venodilator. It makes veins relax, which decreases preload. In a patient with an RV infarct who is already hypotensive and desperate for preload, giving nitro would be catastrophic. His blood pressure would tank. Big no.
C) Administer metoprolol: Beta-blockers are a standard part of STEMI care, but they are an absolute contraindication in a patient who is hemodynamically unstable. You never give beta-blockers to someone who is hypotensive or in heart failure. This is wrong.
D) Perform urgent PCI: This is the definitive treatment. It's what will ultimately fix the problem by opening up the blocked artery. But the patient is unstable. We need to stabilize him first before rushing him to the cath lab. PCI is the end goal, but it’s not the immediate next step.
E) Obtain a chest X-ray: A chest X-ray has its place in a chest pain workup, but it's not going to change our immediate management here. We have a clear STEMI on the EKG. Ordering an X-ray just delays the life-saving interventions this patient needs.
Tutor Tip: The USMLE loves to test contraindications. Recognizing that this patient's hypotension makes both nitroglycerin and beta-blockers dangerous is a key clinical reasoning skill. The second you see an inferior STEMI paired with hypotension, your mind should jump to "RV involvement" and "avoid preload reduction at all costs."
The correct answer is A) Administer intravenous fluids. Stabilizing the patient's blood pressure is the most critical first action. Only then can he safely proceed to definitive reperfusion therapy with PCI. This methodical approach is exactly what separates good scores from great ones, and it's a skill we can absolutely help you master.
Building a Repeatable Question Analysis Framework
Crushing Step 2 CK on exam day isn't about luck. It's about having a reliable, almost second-nature system that holds up under pressure. Just grinding through thousands of USMLE Step 2 CK sample questions won't cut it if you don't know how to break them down.
You need a mental checklist, a consistent method for dissecting every single vignette efficiently and accurately. This is a core strategy we drill into our students at Ace Med Boards because it’s the secret to building the speed and confidence you need to dominate the exam.
The process boils down to a simple, three-part flow: dissect the information, differentiate between the choices, and decide on the best answer.
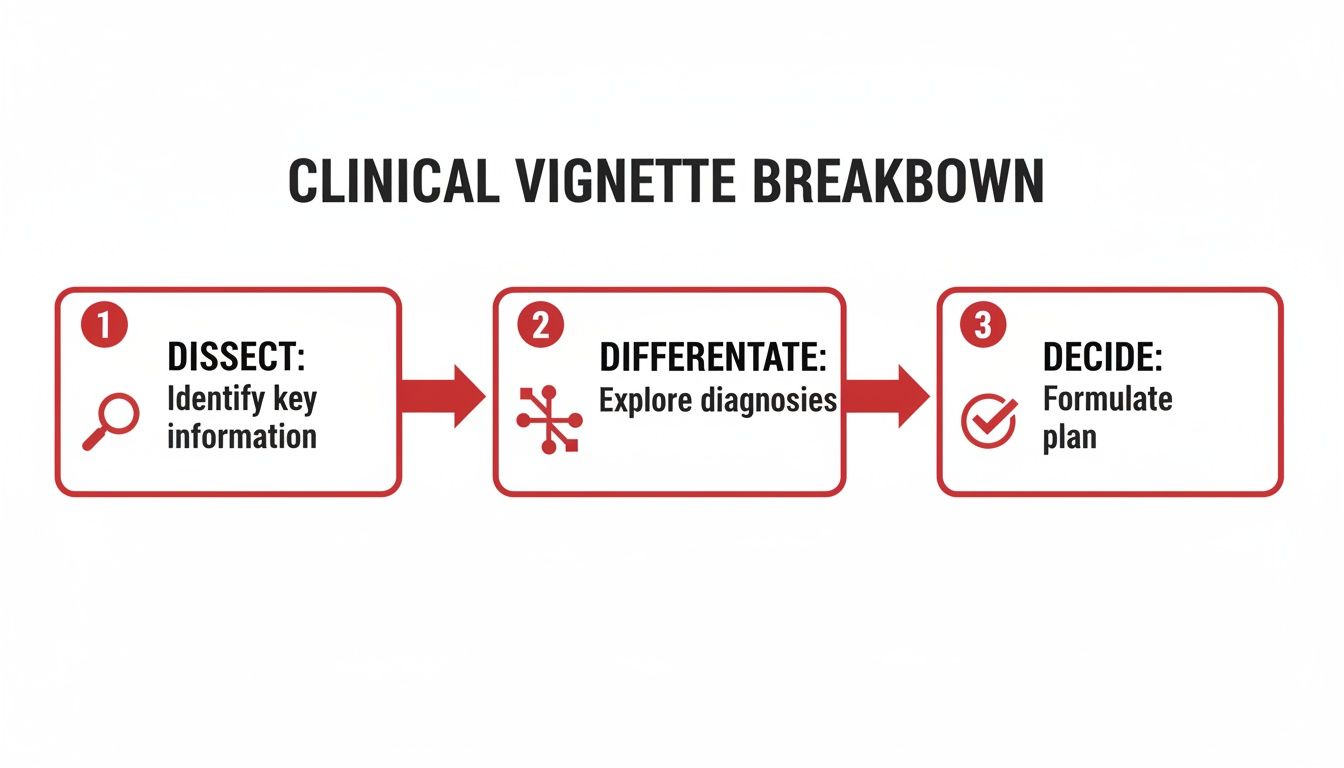
Mastering this flow is what separates a good score from a great one. Let's break down how to turn this into a concrete, step-by-step strategy you can use on every single question.
This table outlines a framework you can apply to any question stem you encounter. It’s designed to be a deliberate, repeatable process that guides your thinking from the first read to the final click.
Strategic Question Analysis Framework
| Phase | Key Action | Example Application |
|---|---|---|
| 1. The Anchor Scan | Read the last sentence first. Identify the chief complaint. | "What is the most likely diagnosis?" + "a 65-year-old man with chest pain." Your brain is now primed to look for diagnostic clues for chest pain. |
| 2. Data Extraction | Scan the vignette for pertinent positives and negatives. | Positive: crushing substernal pain radiating to the jaw. Negative: no JVD, clear lung sounds. This points toward an MI but away from acute CHF. |
| 3. Contextual Analysis | Interpret labs and imaging within the patient's story. | A troponin of 0.03 ng/mL is normal, but in a patient with 20 minutes of chest pain, it doesn't rule out an MI. It just means it's early. |
| 4. Pre-emptive Answer | Formulate your own answer before looking at the options. | Based on the history and EKG showing ST elevations, the diagnosis is an acute STEMI. The next step should be cath lab activation. |
| 5. Evaluate & Eliminate | Compare your pre-emptive answer to the choices provided. | Options A, B, and C are incorrect because they address other conditions. D matches your "cath lab" plan. E is a distractor. Select D. |
By internalizing this structured approach, you turn chaotic vignettes into predictable puzzles. You stop reacting to the question and start controlling it.
Finding Your Anchor: The Initial Scan
Before you get bogged down in the details, do a quick scan. Your first move should always be to read the last sentence—the actual question—and then identify the chief complaint. This simple habit anchors your entire thought process.
Is it a "most likely diagnosis" question? A "next best step in management" question? Or a tricky "mechanism of action" question? Knowing your destination from the start keeps you from wandering down the wrong clinical rabbit hole.
For example, if the question asks for the "next best step," your brain should immediately switch into algorithm mode. You're not just there to diagnose; you're actively making a treatment decision based on the data you're about to read.
Mining for Clues: Extracting Key Data Points
Now you're ready for a more detailed pass. Your goal is to pull out the critical data while consciously ignoring the noise. The NBME writers are experts at packing stems with distractors and irrelevant social history to test your clinical judgment.
Create a quick mental list of these two things:
- Pertinent Positives: These are the classic signs, symptoms, and lab findings that scream a specific diagnosis. Think ST-elevations on an EKG for a patient with crushing chest pain. They're the slam dunks.
- Pertinent Negatives: These are just as crucial. They are the findings you’d expect to see with certain diseases that are conspicuously absent. For instance, clear lung sounds in a patient with an inferior MI helps you push acute left-sided heart failure further down your differential.
This process of gathering positives and negatives is what lets you build a powerful differential diagnosis before the answer choices can bias your thinking. Honing this skill is one of the fastest ways to enhance your test-taking skills and add points to your score.
Putting It All Together: Interpreting Labs and Imaging
Labs and imaging results are never just numbers on a page; they're pieces of the clinical puzzle. You have to interpret them within the context of the vignette. A slightly elevated white count might mean nothing in one patient, but in a post-op patient with a new fever, it's a massive red flag.
Don’t just spot the abnormal values. Ask yourself why they're abnormal and how they fit the story. This contextual analysis is what separates the top-tier scores from the rest.
The real skill isn't just spotting a critical lab value, but immediately understanding its implication for management. A potassium of 6.5 mEq/L isn't a number; it's a medical emergency that demands an EKG and stabilizing treatment, now.
Making the Call: Selecting the Next Best Step
Finally, with your analysis done, you can confidently turn to the answer choices. Because you’ve already built a differential and pinpointed the core clinical problem, you can slice through the options, quickly eliminating those that are obviously wrong or suboptimal.
Your focus should be on the choice that directly addresses the most urgent issue. Is the patient hemodynamically unstable? Prioritize stabilization. Is there a life-threatening diagnosis that needs immediate confirmation? Pick the diagnostic test with the highest yield. This repeatable framework transforms a high-stakes guess into a deliberate, logical, and point-scoring process.
Understanding the Scoring Landscape
Mastering clinical vignettes is the core of your prep, but that effort needs to be aimed at a specific target. Grounding your score goal in the reality of residency admissions isn't just a good idea—it's absolutely essential for building a study plan that actually gets you where you want to go. The numbers tell a story, and you need to listen.
Recent data paints a stark picture of just how critical a solid first attempt is. In the 2023-2024 testing period, 88% of the 14,395 first-time takers passed Step 2 CK. Not bad. But for the 1,411 people repeating the exam, that success rate plummeted to just 60%. The stakes on your first try are incredibly high.
This underscores a simple truth: it is far, far easier to prepare thoroughly once than to navigate the grueling and statistically unfavorable path of a re-take.
The Bar Keeps Getting Higher
With Step 1 now pass/fail, your Step 2 CK score has become one of the most important filters residency programs use. It’s no surprise that this added pressure has pushed the average scores up significantly.
For U.S. and Canadian students, the average score is now floating around 248-250. This is a huge shift. A score that might have been considered fantastic a few years ago is now squarely in the middle of the pack. The entire applicant pool is performing at an incredibly high level.
To be truly competitive, you can't just aim for "average." You have to understand what a "good" score looks like for your specific specialty. If you want to dig deeper, check out our guide to the USMLE Step 2 passing score.
What Your Score Goal Really Means
Your target score isn't just an arbitrary number; it's the key that opens doors to certain specialties. Context is everything here.
- A score of 248 could make you a very strong applicant for Family Medicine.
- However, that exact same score would be seen as less competitive for a specialty like Dermatology or Orthopaedic Surgery, where matched applicants are consistently scoring well into the 250s and even 260s.
Think of your score as a passport. A higher score gives you more stamps and lets you travel to more destinations. Setting a realistic but ambitious goal based on your dream specialty is what will fuel you through the toughest days of studying.
This data-driven approach is precisely why a one-size-fits-all study plan fails. It’s not just about passing the exam; it’s about hitting a score that aligns with your residency dreams. When you understand the competitive landscape, you can tailor your efforts, hammer your weak points, and prep with a clear, strategic purpose.
Connecting Your Score to Competitive Specialties

Let's talk about what your Step 2 CK score actually means. It's more than just a passing number; it's the key that unlocks doors to residency programs. This is where your performance on USMLE Step 2 CK sample questions has a direct, real-world impact on your future. Honestly, setting a specific score goal is one of the best motivators you can have.
Things got a little tougher on July 1, 2025, when the USMLE Management Committee bumped the passing score from 214 to 218. This tweak, combined with the latest match data, tells a very clear story: the score you need varies wildly depending on the specialty you're aiming for.
Setting Realistic Score Targets
You have to look at the data. It's not about finding a hard cutoff, but about understanding the ballpark you need to be in to be a competitive applicant. These numbers give you a solid benchmark for your own prep.
Here’s a snapshot of average scores for matched U.S. MD seniors, based on recent NRMP data:
- Dermatology: 257
- General Surgery: 253
- Emergency Medicine: 248
- Family Medicine: 244
These numbers show exactly why a one-size-fits-all study plan just doesn't work. Someone shooting for Family Medicine has a very different target than someone dreaming of Dermatology. The goal isn't just to pass; it's to land a score that makes program directors notice you. For an even more detailed look, check out our breakdown of Step 2 scores by specialty.
Keep in mind that these are just averages. Top-tier programs in fields like Derm or Plastics often look for applicants well above these numbers, frequently in the 260+ range. Your goal should be to land comfortably within the competitive range, not just scrape by.
Why Personalized Prep Matters
This data-driven reality is precisely why a personalized strategy is so critical. If your target is a 255 or higher, the intensity of your prep, the resources you use, and how aggressively you tackle weak areas have to be on another level compared to someone aiming for a 240.
Personalized guidance is all about bridging the specific knowledge gaps between your current performance and the score your dream specialty demands.
As you line up your Step 2 CK goals with your residency ambitions, it's also smart to keep an eye on the bigger picture. You can explore current market trends for various medical fields to help inform your long-term career path. Ultimately, knowing your target score transforms studying from a general review into a focused, strategic mission.
Your Top Step 2 CK Prep Questions, Answered
Even with the best-laid plans, the Step 2 CK grind brings up questions. It's totally normal. Let's tackle some of the most common ones I hear from students so you can stay focused and confident while you're deep in the Qbank trenches.
How Many Practice Questions Should I Actually Do?
There isn't a single magic number here, but here's what the data and my experience show: most students who crush this exam get through a minimum of 3,000 to 4,000 unique practice questions. Typically, this comes from a top-tier Qbank like UWorld.
But let's be clear—volume alone is not the goal. Simply clicking through thousands of questions won't get you the score you want. The real magic happens in how you review them. You have to meticulously break down every single question, especially the ones you got wrong (and even the ones you got right by guessing!). This is where you dig in to understand the clinical logic and spot the subtle clues you might have missed the first time around.
What's the Best Way to Review Questions?
You need a system, something you do for every single question without fail. It becomes second nature. For every USMLE Step 2 CK sample question, make sure you can:
- Nail the Core Problem: In one sentence, what’s the real clinical issue here? Is it septic shock, an acute MI, or something else? Get to the point.
- Defend the Right Answer: Articulate exactly why the correct choice is the best next step. It's not just about being a good option; it has to be the most appropriate one for this specific scenario.
- Demolish the Distractors: This is critical. Explain precisely why every other answer choice is wrong, not the best choice right now, or even dangerous in this clinical context.
A game-changer for many students is keeping a journal or a simple spreadsheet. Log the concepts you consistently miss. This turns your Qbank from a simple test into your most powerful learning tool. It lets you zero in on your weak spots instead of wasting time re-reading things you already know.
Your Qbank performance isn't just practice; it's a powerful predictor of your future. The data clearly shows a direct link between hitting benchmark scores and successfully matching into competitive fields. Every single question review counts.
Are Practice Exam Scores Really Predictive?
Absolutely. Scores from high-quality self-assessments are typically very good predictors of how you'll perform on the real deal. When you take the NBME Self-Assessments or the UWorld Self-Assessments (UWSA) under timed, exam-like conditions, they give you an honest snapshot of where you stand.
Often, your average score across a few of these exams late in your dedicated study period is within a handful of points of your actual test-day score. This is invaluable data. Just look at the numbers for matched U.S. MD seniors: scores range from an average of 244 in Family Medicine to 257 in Orthopaedic Surgery. Unmatched applicants often score 5-15 points lower. For a deeper dive into how scores correlate with specialty choice, check out the data in the 2025 NRMP Charting Outcomes.
Feeling like you're drowning in questions or just need a more structured way to tackle your weaknesses? The expert tutors at Ace Med Boards live for this stuff. We specialize in building personalized study plans that turn those weak areas into your biggest strengths. Schedule your free consultation today!
