The path to residency starts long before you even see the ERAS portal. The groundwork you lay during your third and early fourth year is your secret weapon for a less stressful, more successful application season. Think of this time as building the entire frame of your application—get it right, and everything else falls into place.
Building Your Foundation in Third and Fourth Year
Let's be clear: the residency application timeline doesn't really kick off when the software opens. It starts with the strategic moves you make during your third and early fourth years of med school. This period is less about filling out forms and all about building the actual substance of your application.
Your main focus here should be twofold: clinical performance and relationship building. Every single rotation is an opportunity to learn, yes, but it’s also a prime chance to identify mentors and the people who will write you stellar letters of recommendation. The stories and experiences you collect now will become the fuel for your personal statement and the core of your interview answers later on.
Strategically Scheduling Your M4 Year
How you structure your fourth year can make or break your application. The goal is to front-load your Sub-Internships (Sub-Is) and key electives, ideally scheduling them between June and October. This timing is crucial for two reasons: it allows you to lock in powerful Letters of Recommendation (LORs) from attendings in your chosen specialty, and it gives you fresh, relevant experiences to talk about in your interviews.
When you're mapping it all out, keep this in mind:
- Home vs. Away Rotations: Schedule a Sub-I at your home institution early on. It's the best way to get a guaranteed, strong LOR. Use away rotations to check out programs high on your list, but be warned—they are competitive and often require separate applications months in advance.
- Specialty-Specific Electives: Prioritize rotations that directly beef up your application for your target specialty. An aspiring surgeon, for instance, should be scheduling rotations in surgical subspecialties or critical care.
- Lighter Rotations Later: Save your less demanding rotations for the peak of interview season (roughly October through January). This will give you the flexibility you need for travel and prep without falling behind.
Securing Powerful Letters of Recommendation
A truly compelling LOR isn't just a summary of your performance; it tells a story about your clinical skills, work ethic, and personality. The process of getting these letters needs to start months before the deadline. Pinpoint attendings you've worked with closely, especially those who have seen you shine in challenging situations.
The perfect time to ask is right at the end of a successful rotation, while your excellent performance is still fresh in their mind. Don't be casual about it—make it a formal, professional request.
Pro Tip: When you ask for a letter, hand your attending a packet containing your CV, a draft of your personal statement, your ERAS photo, and the AAMC's LOR request form. This makes their job infinitely easier and helps them write a much more detailed, personalized letter for you.
Juggling all these tasks requires some serious organizational skills. Many students find it helpful to explore effective time management schedules to keep everything on track. This groundwork isn't just about checking boxes; it’s about building a compelling narrative of your dedication. For example, a strong research background can be a huge differentiator. Check out our guide on how medical student research can build a competitive residency application for a deeper dive.
Solidifying Your Specialty and Finding Mentors
While some students walk into med school knowing exactly what they want to do, most use their third-year rotations to figure it out. As you head into your fourth year, it's time to make a decision. This choice will shape everything—your electives, your research focus, and the entire narrative of your personal statement.
Start seeking out faculty and residents in your field of interest for advice. A good mentor is worth their weight in gold; they can review your application, offer candid advice, and even make introductions at programs you're targeting. Their insight into the field's competitiveness is also invaluable.
For instance, understanding the match statistics is key to forming a smart strategy. U.S. medical graduates (both MD and DO) enjoy a high overall match rate of about 94.2%. But the picture is different for International Medical Graduates (IMGs), where U.S. citizen IMGs match at around 70.1% and non-U.S. citizen IMGs at 58.3%, often due to visa hurdles and specific program preferences. Getting familiar with these numbers helps you set realistic expectations and build the right application strategy.
Mastering the Core Application Season from June to September
If the residency application cycle is a marathon, the stretch from June to September is the all-out sprint to the finish line. This is where all your hard work starts coming together into the application that programs will actually see. Every single action you take during these four months can directly impact your chances of matching.
It all kicks off with something small but powerful: your ERAS token.
Most medical schools release these tokens in June. This is your golden ticket into the Electronic Residency Application Service (ERAS), where you'll register and begin the painstaking process of building your application. Don't underestimate how long this takes. This isn't just data entry; it's about carefully crafting a compelling story about who you are and why you're a great fit for your chosen specialty.
Kicking Off the Application in June
Once you've registered on MyERAS, your first job is to start chipping away at the application itself. Think of it as your professional autobiography. It’s where you’ll detail your work, volunteer, and research experiences to showcase your growth and dedication.
Get specific when describing your activities. A vague entry like "Volunteered at a free clinic" doesn't do you justice. Instead, try something like, "Coordinated patient triage and managed intake for over 20 non-English speaking patients weekly, improving clinic workflow and patient communication." See the difference? One is a task, the other is an impact.
A Quick Note on Experiences: Program directors value quality over quantity. A few deeply meaningful experiences with thoughtful, reflective descriptions will always beat a long laundry list of activities where you barely scratched the surface. They want to see genuine commitment.
At the same time, you should be neck-deep in writing and refining your personal statement. This one-page essay is your only chance to speak directly to the people who will decide your future. It needs to tell a story that connects the dots between your past experiences and your passion for your chosen field.
Don't just rehash your CV in paragraph form. Pick two or three key moments and weave them into a narrative that reveals your personality, resilience, and unique qualities. Get feedback from mentors, advisors, and trusted peers, but make sure the final version still sounds like you.
This is also the time when exam scores and application work start to collide. Juggling everything is a huge challenge.
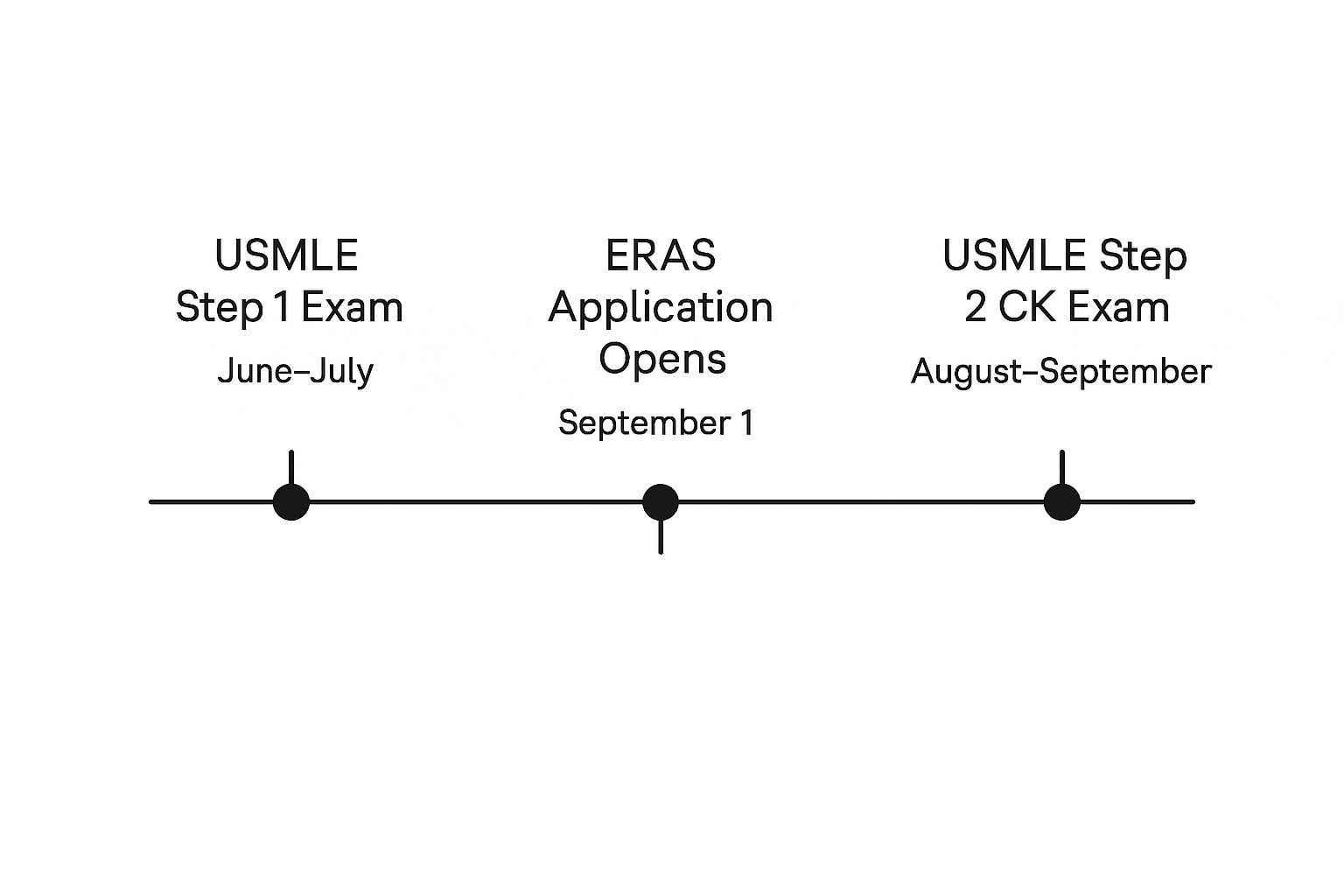
As you can see, the window for taking key exams like USMLE Step 2 CK often overlaps directly with the most intense application prep period, making time management absolutely critical.
The Document Chase: July and August
As summer heats up, your focus needs to shift to chasing down all your supporting documents. This requires polite but persistent follow-up.
- Letters of Recommendation (LORs): You should have already asked for your letters by now. July and August are for confirming that your letter writers received the Letter Request Form from MyERAS and gently reminding them of the September submission deadline.
- Medical School Performance Evaluation (MSPE): Your medical school handles uploading the MSPE, often called the "Dean's Letter." It’s a good idea to check in with your student affairs office to know their internal timeline and see if they need anything else from you.
- Transcripts: You'll need to get both your medical school transcript and your USMLE transcript sent to ERAS. You can authorize the release of your USMLE scores right in the portal, and you'll need to confirm with your registrar that your academic transcript has been uploaded. Our in-depth guide on the full ERAS application timeline has a handy checklist for these items.
As you navigate this period, having a clear, high-level view of your tasks can prevent things from falling through the cracks. This table breaks down the essential action items month by month.
Key ERAS Application Milestones from June to September
This table summarizes the critical tasks and deadlines from June to September. Use it as a quick-reference guide to stay organized and on track during the busiest part of the application season.
| Month | Key Action Items | Strategic Tip |
|---|---|---|
| June |
- Receive and register your ERAS Token.
- Begin filling out the MyERAS application sections.
- Draft and refine your Personal Statement. | Start describing your most significant experiences first while the details are fresh. Aim for a completed first draft of your personal statement by the end of the month. |
| July | - Continue working on the ERAS application.
- Send polite reminders to LOR writers.
- Authorize release of your USMLE transcript. | Finalize your program list and start tailoring your personal statement for specific programs or specialties if needed. This is the month for diligent, consistent work. |
| August | - Finalize and proofread all application sections.
- Confirm LORs have been uploaded.
- Ensure MSPE and transcript are submitted by your school. | Do a full, top-to-bottom review of your application with a trusted mentor or advisor. Check for consistency, clarity, and typos. This is your last chance for major edits. |
| September | - Perform final review of the entire application.
- Certify and submit your application to programs.
- Prepare for interview invitations. | Submit on day one. Programs get flooded with applications. Being in the first wave they see is a significant advantage. Don't wait until the last minute. |
Staying on top of these milestones will put you in a strong position when the submission window opens, reducing stress and increasing your chances of success.
The September Submission Strategy
September is go-time. While ERAS lets you start certifying and submitting your application early in the month, program directors can't actually see anything until a specific date later in September.
There is a massive strategic advantage to submitting your application so it's ready for programs the very first day they can view it. They are immediately swamped with thousands of applications. Submitting early ensures you’re in that first batch they review. Waiting even a day or two can mean your file gets buried under hundreds of others that came in first.
This is especially critical in competitive specialties where application numbers are climbing. For instance, Internal Medicine saw its applicant pool grow by 5%. That trend was even more dramatic for International Medical Graduates (IMGs), whose applications to Internal Medicine jumped by 5.2%. Family Medicine also saw an 8.1% rise in total applicants, with IMG applications surging by an incredible 13.3%. With competition this fierce, an early, polished submission is non-negotiable.
Before you hit that final "Certify & Submit" button, do one last, exhaustive review. Read every word. Once you certify, most sections are locked for good. It’s the point of no return, so make it count.
Navigating Interview Season From October To January
Once your application is in, the game changes. The long marathon of preparation is over, and now it's all about performance. Welcome to interview season, the whirlwind period from October to January that's defined by a constantly buzzing phone, a perpetually refreshing inbox, and the challenge of being your best self for program after program.
This phase is all about speed and readiness. Interview invitations can start trickling in the very first day programs get your application (often late September), but the real floodgates open from October through December. They can land at any time—day or night—and you'll quickly learn that popular programs fill their limited interview slots within hours. Being ready to jump on an invitation immediately is a massive advantage.

Mastering The Invitation And Scheduling Process
The second an invitation hits your inbox, the clock starts ticking. Your goal is simple: lock in a date as fast as humanly possible. This isn't just about securing a spot; it's about showing the program you're organized, enthusiastic, and that they are a priority for you.
Here's how to handle the chaos like a pro:
- Set Up Alerts You Can't Ignore: Turn your email notifications on and make them loud. I've known applicants who set a unique, blaring ringtone just for ERAS-related messages so they never miss one.
- Respond Within 24 Hours—Minimum: A fast reply is non-negotiable. Even if you need a moment to sort out your schedule, a quick acknowledgment shows you're engaged. Ideally, you should be accepting and scheduling within a few hours.
- Use a Centralized Calendar: The moment you confirm a date, block it off in your calendar. Don't forget to include pre-interview social events and travel time. A shared digital calendar like Google Calendar is your best friend here—it's the easiest way to avoid the common, and very stressful, mistake of double-booking yourself.
Juggling multiple offers gets tricky. What if your top-choice program offers a date that conflicts with an interview you've already scheduled? Handle it with grace. Politely email the program coordinator of the lower-priority program, reaffirm your strong interest, and simply ask if any alternative dates might be available. Most coordinators get it; they know you're managing a complex puzzle.
Pro Tip: Treat every single interaction with a program coordinator with the utmost respect and professionalism. They are the gatekeepers of the entire process and often have a surprising amount of influence on how an applicant is perceived.
Excelling In Virtual And In-Person Interviews
While the pandemic made virtual interviews the norm, some programs are bringing back in-person or hybrid options. Honestly, the format doesn't matter as much as your preparation. This is where you set yourself apart. You have to go way beyond just reciting your CV; your real goal is to tell a compelling story about who you are and the kind of physician you're going to be.
Great interview prep has layers. It's not just about what you say, but how you say it and what you ask in return. For a much deeper dive, our guide on medical residency interview preparation is packed with specific strategies and practice questions to help you truly shine.
Common Questions You absolutely Must Master:
- "Tell me about yourself." This is not an invitation to read your CV aloud. You need a polished, one-minute narrative that connects your key experiences to your specialty choice and explains what you're looking for in a residency.
- "Why are you interested in our program?" Do your homework. Seriously. Talk about specific things that excite you—a unique rotation, a particular faculty member's research, a community clinic they run. Generic answers are incredibly easy to spot and are a major red flag.
- "Describe a challenging clinical experience." Pick a real story that shows off your problem-solving skills, your resilience, and—most importantly—your ability to learn from tough situations. The focus shouldn't be on the challenge itself, but on what you did and what you took away from it.
Asking Insightful Questions
Remember, the interview is a two-way street. The questions you ask are just as important as the answers you give. They show how engaged you are and what you truly value in a training environment. Whatever you do, don't ask something you could have easily found on their website. It just signals a lack of preparation.
Instead, focus on questions that get to the heart of the program's culture.
- "What's the biggest change the program has gone through in the last couple of years?"
- "What do residents typically do for fun together when they're not in the hospital?"
- "Could you tell me a bit about the mentorship structure for junior residents?"
Following Up With Professionalism
Your professionalism doesn't end when the interview does. Sending a thank-you note is a simple but critical final step. And yes, email is perfectly fine and what most programs expect these days.
Aim to send personalized thank-you notes within 24-48 hours to the program director and any other faculty or residents who interviewed you. Make it memorable by referencing a specific point from your conversation. This small gesture reinforces your interest and leaves one last, positive impression as this crucial phase of the timeline comes to a close.
The Final Stretch to Match Week
After the whirlwind of applications and interviews, the period from January to March feels… strange. It's a mix of intense, stomach-churning anxiety and long stretches of quiet waiting. This is it—the culmination of your entire medical school journey and the final sprint to the single most important week of your career so far. Your focus is no longer on impressing programs; it's on making the critical decisions that will define the next chapter of your life.
Everything now boils down to one of the most nerve-wracking parts of the whole timeline: the Rank Order List (ROL). This is where you officially tell the National Resident Matching Program (NRMP) what you really want. The deadline to certify your ROL is usually in early March, and let me be clear: this is a hard stop. You can't make changes after this date, so give this process the careful, deliberate thought it deserves.
Crafting Your Rank Order List
The single most important rule for creating your ROL is simple, yet applicants agonize over it every single year: rank programs based on your true, genuine preference. That's it. Do not try to "game the system." Don't rank a program higher because you think you have a better shot there, and don't put a "safety" school above your dream program.
The NRMP Match algorithm is actually designed to work in your favor. It starts by trying to place you at your number one choice. If that doesn't work out, it moves to number two, then three, and so on down your list. It's a mathematical process that rewards honesty.
The NRMP algorithm is applicant-proposing, which means it prioritizes your preferences. Ranking a program highly does not hurt your chances at other programs you ranked lower. Your list should be a direct reflection of where you would be happiest training for the next several years.
Think about it this way: if you rank Program B higher than your dream Program A because you think it's more "realistic," and you end up matching at Program B, you'll always wonder. You will never know if you would have matched at Program A had you just been honest with your list. Trust the process and rank with both your heart and your head.
As you sit down to finalize your list, really think about these factors:
- Program Culture: Where did you feel like you belonged? Could you genuinely see yourself thriving with those residents and faculty for the next three to seven years?
- Geographic Location: Be honest about proximity to family, the cost of living, and whether you're a big city person or prefer a smaller town.
- Training Quality: Reflect on the clinical training, the research opportunities, and the fellowship placement rates you saw during your interviews.
Understanding Match Week Dynamics
Match Week, which hits in mid-March, is a highly structured and incredibly emotional week. It's not just one day; the news unfolds in a specific sequence that every applicant needs to be prepared for.
- Monday of Match Week (10 a.m. ET): You'll get an email telling you whether you matched. The email is simple: "Congratulations, you have matched!" or "We are sorry, you did not match." Crucially, it will not tell you where you matched.
- Monday to Thursday: For applicants who didn't match, this is when the Supplemental Offer and Acceptance Program (SOAP) kicks off. It's a frantic, four-day process where unmatched applicants can apply to residency positions that went unfilled.
- Friday of Match Week (12 p.m. ET): This is the famous Match Day. This is the moment when matched applicants finally learn where they will be spending their residency. Most medical schools hold festive, in-person ceremonies to celebrate.
The entire system is only getting more competitive. The Main Residency Match recently became the largest in its 73-year history, with 43,237 positions offered—a 4.2% jump from the year before. This growth included a significant rise in primary care spots, showing how the system is trying to meet healthcare demands. The number of applicants also climbed to 52,498, with the overall match rate for PGY-1 spots holding steady and competitive. These numbers show just how high the demand is and why every step on this timeline is so critical. You can learn more about what the latest Match Day numbers reveal about residency trends.
Preparing For Any Outcome
The emotional weight of Match Week is immense. It’s the moment where years of hard work, sacrifice, and dedication finally come to a head. Whether you match at your top choice or find yourself navigating the SOAP, it is absolutely essential to have a support system ready. Talk with your family, your friends, and your mentors beforehand.
No matter the outcome, Match Day is a monumental achievement. It marks your official transition from student to physician. You've earned this, so make sure you celebrate this incredible milestone.
Preparing for Day One of Residency
That feeling on Match Day when you open the envelope? It’s a career-defining moment. But the residency application timeline doesn’t stop there—it just shifts gears into a frantic administrative phase. Between March and your first day as a resident in July, you're looking at a mountain of paperwork and logistical hurdles that demand your full, immediate attention.
This is the transition from medical student to licensed, employed physician. Get ready for a flood of onboarding documents, contracts, and requests from your new program. Procrastination is your enemy here. Many of these tasks have hard deadlines that can derail your start date if you miss them. Do yourself a favor: create a dedicated folder and a detailed checklist right away.

Navigating Credentialing and Licensing
Before you can even think about seeing a patient, you have to be properly credentialed by your hospital and licensed by the state medical board. This is often the biggest time-sink of the entire post-match process, sometimes taking a full 2-3 months to wrap up.
The paperwork is intense and requires absolute precision. You'll be providing exhaustive details about your education, training history, and personal background. Start gathering these key documents now.
- State Medical License Application: This is its own beast—a separate, often lengthy application that requires notarized documents and official transcripts. Jump on this immediately.
- DEA Registration: You can't prescribe controlled substances without it. You'll need to apply for your Drug Enforcement Administration (DEA) number.
- National Provider Identifier (NPI): Getting your NPI is pretty straightforward, but it's a non-negotiable step for billing and identification purposes.
- Background Checks: Prepare for multiple criminal background checks and fingerprinting requests, usually from both the hospital and the state board.
For international medical graduates on a tight schedule or facing unexpected hold-ups, learning about expediting your US visa appointment can be a lifesaver. Any delay in this administrative maze can jeopardize your start date.
A rookie mistake is underestimating how long it takes third parties to send documents. Request transcripts and letters of good standing from your medical school way ahead of time, and then follow up to make sure they were actually sent.
Managing Relocation and Finances
On top of all the paperwork, you've got the very real challenge of moving to a new city, probably on a shoestring budget. If you haven't already, start researching neighborhoods and housing options the second you match. Many programs have internal message boards or resident forums that are goldmines for advice on where to live.
This transition can also be a financial pressure cooker. You’ll have moving expenses and security deposits to pay long before you see your first paycheck. It’s a smart move to map out a detailed budget for these months. Many residents end up taking out a small relocation loan to bridge the gap, which helps them get settled without constant money stress.
Preparing Mentally for Intern Year
Finally, and this is critical, take some time for yourself. The months leading up to residency are the last real break you’ll have for a long time. Burnout is a massive issue in medicine. Starting intern year well-rested and mentally centered is one of the best gifts you can give your future self—and your future patients.
Spend quality time with family and friends. Travel if you can. Reconnect with your hobbies. You’ve conquered the grueling medical residency application timeline and earned this moment. Arriving on day one with a clear head and a solid plan is the final, crucial step to launching a successful career.
Common Questions About the Residency Timeline
The residency timeline is a beast. Even with a perfect month-by-month plan, you're going to have questions pop up. It's a high-stakes process, and getting clear answers can be the difference between feeling confident and feeling completely overwhelmed.
Let's tackle some of the most common questions we hear from applicants every single year. This isn't just generic advice; it's based on years of guiding students through the Match successfully.
How Many Residency Programs Should I Apply To?
This is the big one, and the honest answer is: it depends. There’s no magic number here. The right amount hinges on how competitive your chosen specialty is and, frankly, how strong your application is.
For the ultra-competitive fields—think dermatology, neurosurgery, or ortho—it's not uncommon for applicants to apply to 40-60+ programs. On the other hand, if you're a strong candidate for a less competitive specialty like family medicine or pediatrics, 20-30 programs might be plenty.
Here’s how to think about building your list:
- Dig into the Data: The NRMP publishes "Charting Outcomes in the Match" data every year. This is your bible. It shows you exactly how many programs matched applicants in your specialty applied to. Start there.
- Build Your Tiers: Don't just apply to the top 10 programs in the country. A smart list has a healthy mix of "reach" (your dream programs), "target" (where you're a good fit), and "safety" (where you're a very strong candidate) schools.
- Talk to Your Advisor: Your specialty advisor has seen this movie before. They know the landscape and can give you personalized advice based on your scores, research, and letters.
A strategic approach is always better than the scattergun method. It will save you a ton of money on application fees and, more importantly, prevent interview burnout later in the season.
When Should I Take the USMLE Step 2 CK?
The ideal timeline has your USMLE Step 2 CK score back before residency programs can start viewing your ERAS application in late September. With Step 1 now pass/fail, your Step 2 score has become one of the most critical objective filters programs use. A great score can make your application.
Most students aim to take the exam in the late spring or early summer—think May to July—before application season kicks into high gear. This timing is strategic. It gives you a dedicated study block that doesn't overlap with demanding sub-internships, allowing you to crush both.
Waiting until August or later is playing with fire. It's possible, sure, but a score delay could mean programs review your application without that key data point. That immediately puts you at a disadvantage compared to everyone else with a complete file.
Do I Really Need to Do the Supplemental ERAS Application?
If you're applying to a specialty that uses it, the answer is an emphatic yes. The Supplemental ERAS Application isn't really "supplemental" anymore; it's essential.
This is your chance to give programs more context. You can signal your genuine interest, explain your geographic preferences, and really highlight your most meaningful experiences. Programs are sorting through thousands of applications, and they use this data to find the applicants who are a serious fit.
Skipping it sends a bad signal. It can look like you’re not serious about their program or just aren't on top of the process. Either way, you risk getting filtered out before a real person even sees your file. Always check the AAMC website early to see which specialties are participating that year.
How Do I Handle Conflicting Interview Offers?
First off, this is a great problem to have! But you need to handle it with professionalism and speed. Communication is everything.
You should respond to every single interview invitation within 24-48 hours. Even if you're just acknowledging you received it while you check your calendar, a prompt reply shows respect.
If you have a direct conflict, politely email the program coordinator. Reiterate your strong interest in their program and ask if there’s any chance of an alternative date. Most coordinators are used to this and are incredibly helpful; they might have a waitlist for interview slots or find a way to be flexible.
Whatever you do, don't be a no-show or cancel at the last minute unless it's a true emergency. It reflects poorly on you and on your medical school.
Navigating the complexities of board exams and residency applications can be challenging, but you don't have to do it alone. At Ace Med Boards, our expert tutors provide personalized one-on-one guidance to help you excel on your USMLE exams and build a standout application. Learn more about our approach.
