When a patient comes to you with a cough and a fever, what's the first thing that pops into your head? The flu? A common cold? Pneumonia? Maybe something less common?
The mental process you just went through is the beginning of a differential diagnosis. It’s the methodical approach clinicians use to tell one disease from another when they share similar signs and symptoms. This isn't just about making a list; it's a dynamic skill of sorting through possibilities to land on the most likely answer.
Think of it as disciplined medical detective work. It’s the absolute bedrock of sound clinical reasoning.
The Art of Medical Detective Work
Crafting a differential diagnosis is far more than just rattling off a list of potential illnesses. It's a structured process of gathering clues from the patient's history, physical exam, and lab results, weighing the evidence for each possibility, and systematically ruling things out.
This framework is what allows a doctor to move from a wide-open field of potential causes to a short, actionable list of probabilities. It’s how you navigate clinical uncertainty safely and effectively.
Why This Process Is So Critical
You simply can't overstate the importance of a structured diagnostic approach. Getting the diagnosis wrong can lead to the wrong treatment, causing real harm. By methodically considering multiple possibilities, clinicians sidestep cognitive biases, like jumping to the first conclusion that fits.
This systematic practice ensures that:
- You don't miss the big stuff. It forces you to consider serious but less common conditions that could be disastrous if overlooked.
- Patient safety comes first. A thorough evaluation prevents you from closing the case too early and missing the real culprit.
- Treatment actually works. An accurate diagnosis is the essential first step toward effective therapy.
This systematic approach is the backbone of modern medicine. The term first appeared in Herbert French's 1913 book, "An Index of Differential Diagnosis of Main Symptoms," formally cementing its place in medical practice. You can dig into its history on the National Library of Medicine website.
Building Your Foundation for Success
For any medical student, mastering this skill is non-negotiable, especially when you're staring down high-stakes board exams. A rock-solid grasp of what is differential diagnosis is your best weapon for dissecting complex clinical vignettes.
This is where you move beyond rote memorization and start developing true clinical reasoning. Honing this ability is a massive part of figuring out how to study for USMLE Step 1 and other board exams. It’s what transforms your textbook knowledge into a practical tool for solving real-world patient problems.
To give you a clearer picture, here's a quick breakdown of the core components.
Key Components of Differential Diagnosis at a Glance
This table breaks down the core elements of the differential diagnosis process for a quick, digestible summary.
| Component | Description | Clinical Example |
|---|---|---|
| Initial Clue Gathering | Collecting data from the patient history, physical exam, and initial observations. | A 55-year-old male presents with chest pain. History reveals smoking and hypertension. |
| Generating Possibilities | Brainstorming a broad list of potential diagnoses based on the initial presentation. | Could be myocardial infarction, pulmonary embolism, GERD, costochondritis, or aortic dissection. |
| Prioritizing the List | Ranking the potential diagnoses from most to least likely, often focusing on the most life-threatening conditions first. | Myocardial infarction and pulmonary embolism are prioritized due to their immediate life-threatening nature. |
| Systematic Rule-Out | Using further tests, imaging, and clinical findings to confirm or eliminate possibilities from the list. | An EKG and troponin levels are ordered. A normal EKG and negative troponins make MI less likely. |
| Refining the Diagnosis | Narrowing down the list to a final working diagnosis or a very short list of likely candidates. | With a negative cardiac workup, the focus shifts to GERD or musculoskeletal causes. |
| Final Confirmation | Establishing the definitive diagnosis, which guides the final treatment plan. | A trial of proton pump inhibitors resolves the pain, confirming a diagnosis of severe GERD. |
Ultimately, mastering the differential diagnosis is what separates the novices from the expert clinicians and forms the very foundation of excellent patient care.
A Four-Step Framework for Diagnostic Clarity
How do you get from a patient's story to the right diagnosis? Without a repeatable method, it’s all too easy to get lost in a sea of possibilities or, even worse, jump to the wrong conclusion. The differential diagnosis process is that essential framework—a reliable blueprint for navigating any clinical puzzle you encounter.
Think of it as a logical, four-stage progression that methodically transforms raw patient data into a clear, actionable diagnosis.
This process isn't a single "aha!" moment. It's a deliberate sequence of narrowing down the options based on evidence.
Let's break down how this works, step by step.
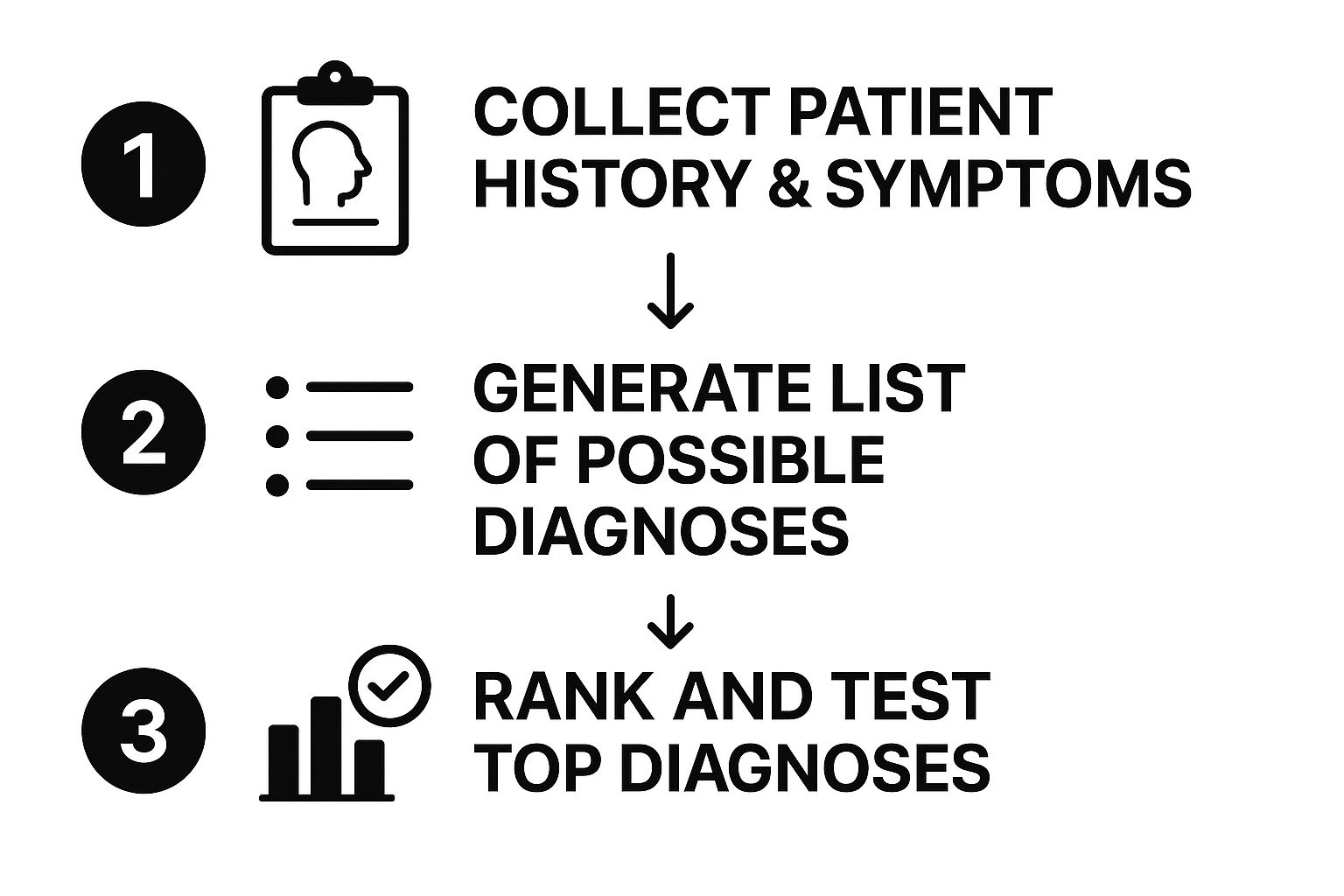
Step 1: Gather Your Clues
The first step is pure detective work. You’re collecting every piece of available information from the patient's history, a thorough physical exam, and your initial observations. This phase is all about listening intently and observing carefully to pick up on the details that will steer your thinking.
Every bit of data—from when the symptoms started to the patient’s social history—is a potential clue. This foundational work sets the stage for everything that comes next.
Step 2: Build a Comprehensive List
With your initial clues in hand, you can start brainstorming a list of every potential cause. At this stage, you want to cast a wide net. Consider everything that could plausibly explain the patient’s presentation, from the most common conditions to the rare-but-serious ones.
Using mnemonics can be a huge help here. For example, the "I VINDICATE" mnemonic helps you remember different categories of disease (Idiopathic, Vascular, Infectious, Neoplastic, etc.), ensuring you don’t overlook a major category.
The key is to generate a list that is broad enough to include the unlikely but dangerous diagnoses, yet focused enough to be manageable. This is where clinical knowledge and strong study habits converge.
Step 3: Prioritize and Rank Possibilities
Not all potential diagnoses are created equal. The next crucial step is to organize your list, a process often called triage. You need to rank the possibilities based on two key factors: likelihood and severity.
- Most Likely Diagnosis: Given the patient's age, risk factors, and symptoms, what’s the most probable cause?
- Must-Not-Miss Diagnoses: Are there any life-threatening conditions on your list that need to be ruled out immediately, even if they aren't the most likely?
This is the mental sorting that happens as a broad list gets refined into a prioritized set of hypotheses. This clinical judgment—the ability to distinguish the probable from the perilous—is a skill that sharpens with experience and dedicated study. To get ahead, many students rely on focused medical exam study tips to master this type of clinical reasoning for their boards.
Step 4: Refine and Test Your Hypotheses
Finally, you move from thinking to acting. You use targeted tests and further evaluations to confirm or rule out your top hypotheses. This is where you might order specific blood tests, imaging studies, or other diagnostic procedures designed to give you definitive answers.
Each test result is a new piece of evidence that helps you cross possibilities off your list and zero in on the final diagnosis. This iterative process of testing and refining continues until you arrive at a conclusion that is strongly supported by the evidence, leading you to a confident and effective treatment plan.
Bringing the Diagnostic Process to Life
Theory is one thing, but seeing the differential diagnosis process in action is where the lightbulb really goes on. Let’s walk through a classic, high-stakes scenario you'll absolutely face on your exams and in the real world: a patient presenting with acute chest pain. This example shows exactly how a clinician uses the four-step framework to cut through the uncertainty and land on a clear diagnosis.
Imagine a 58-year-old man walking into the emergency department. He's pale, sweating, and complaining of a severe, crushing pain in his chest that started an hour ago. Right there, the diagnostic clock starts ticking. Loudly.
Step 1: Gathering the Initial Clues
The first priority is to gather crucial information—fast. While a nurse gets vital signs, the physician starts firing off targeted questions.
- History of Present Illness: The pain is a 10/10, smack in the center of his chest, and it’s radiating down his left arm. He’s also nauseous and feels short of breath.
- Past Medical History: He has a history of hypertension and high cholesterol, but he admits he isn't great about taking his medication.
- Social History: He's a long-time smoker—one pack a day for 40 years—and has a high-stress job.
- Physical Exam: His heart is racing at 110 bpm, and his blood pressure is jacked up at 160/95 mmHg. His lungs, however, sound clear.
These initial clues are already waving massive red flags for a serious cardiac event.
Step 2: Building the Broad List of Possibilities
With that initial data, the clinician’s mind starts generating a list of potential culprits. This list has to be broad, especially including the deadliest possibilities first.
The core of a strong differential diagnosis is considering both the common and the catastrophic. You have to ask, "What is most likely?" and, just as critically, "What's the worst thing this could be?"
Based on his presentation, the initial differential diagnosis list looks something like this:
- Myocardial Infarction (Heart Attack): This is highly likely given his risk factors and classic symptoms. It's at the top of the list for a reason.
- Pulmonary Embolism (PE): A blood clot in the lungs can absolutely cause chest pain and shortness of breath.
- Aortic Dissection: A tear in the aorta is rare, but it's a catastrophe you can't afford to miss.
- Gastroesophageal Reflux Disease (GERD): Never underestimate severe heartburn; it can mimic cardiac pain surprisingly well.
- Costochondritis: Inflammation where the ribs meet the sternum—a musculoskeletal cause.
- Panic Attack: Can present with chest tightness, a racing heart, and a feeling of doom.
Step 3: Prioritizing and Ranking the Diagnoses
Next comes the mental triage. The clinician has to rank this list based on a blend of severity and probability. What's going to kill him first?
- Myocardial Infarction is locked in at the number one spot. It’s the most probable diagnosis and demands immediate action.
- Pulmonary Embolism and Aortic Dissection are the "must-not-miss" diagnoses. They might be less common, but they're true medical emergencies.
- GERD, Costochondritis, and Panic Attack are shuffled to the bottom. They are less likely and far less dangerous, but they stay on the list for now.
Step 4: Refining With Targeted Tests
The final step is all about using diagnostic tests to prove or disprove the top contenders on the list. This is where you move from suspicion to certainty.
An immediate electrocardiogram (ECG) is performed, and it shows ST-segment elevations—a classic sign highly suggestive of a heart attack. At the same time, blood is drawn to check for cardiac enzymes (troponins), which are expected to be elevated. These results provide powerful evidence to rule in myocardial infarction.
With that confirmation, the broad differential diagnosis collapses into a single, definitive working diagnosis. The team can now confidently rush the patient for life-saving treatment for a heart attack. This is the process in a nutshell—a systematic journey from a wide range of possibilities to a precise action plan that leads directly to effective patient care. As technology evolves, so do these methods; you can read more about the growing impact of AI for Medical Diagnosis.
Avoiding Common Diagnostic Traps
Even the sharpest clinicians can fall into mental traps that lead to diagnostic errors. Truly mastering differential diagnosis isn't just about building a list of possibilities; it’s about recognizing the cognitive shortcuts that can send you down the wrong path. Bringing these pitfalls into the light is the first step to avoiding them, especially when you're under pressure.
These traps, often called cognitive biases, are just the brain's natural way of trying to simplify a ton of complex information. They're usually efficient, but in medicine, they can be dangerous, leading to a missed diagnosis or the wrong one entirely. Think of this as building up your intellectual self-defense.
Let's break down two of the most common diagnostic traps you'll face on exams and in the clinic.
The Pitfall of Premature Closure
Premature closure is the classic mistake of jumping to a conclusion. It happens when you accept a diagnosis before you’ve actually proven it, stopping your investigation way too early just because a patient’s story seems to fit a familiar pattern.
Here’s a textbook example: a young, anxious-looking patient comes in with a racing heart and shortness of breath. The team quickly labels it a panic attack and starts talking about discharge. They've fallen for premature closure by failing to rule out a deadly pulmonary embolism, which can look almost identical at first glance.
The antidote is simple but incredibly powerful: always ask, "What else could this be?" Forcing yourself to finish the diagnostic process, even when the answer feels obvious, is one of the most important safety checks in medicine.
The Influence of Availability Bias
Availability bias is what happens when a recent or particularly dramatic case sticks in your mind and skews your judgment. If you’ve just seen three straight cases of the flu, you’re much more likely to diagnose the fourth patient with a cough as having the flu, too, even if their symptoms don't quite line up. That flu diagnosis is just more "available" in your brain.
Imagine an ER doc who just dealt with a harrowing case of aortic dissection. For the next few weeks, they might find themselves ordering extensive, invasive workups for every patient with chest pain, even when it’s far more likely to be simple muscle strain. That one rare but memorable case is clouding their ability to assess a common one.
The way to fight this is to consciously ground yourself in the objective data from the patient in front of you, not the ghosts of patients past. This kind of mental discipline is vital, especially when exam stress makes you want to take shortcuts. It's also why staying mentally well is so important; recognizing the signs of burnout is a huge part of protecting your clinical judgment. You can learn more about managing USMLE exam burnout to keep your mind sharp.
By actively looking for these biases in your own thinking, you can build cognitive guardrails that protect your reasoning and ensure you're providing the safest, most effective care possible.
Adapting Your Approach in Specialized Fields
The core principles of differential diagnosis hold true everywhere, but how you apply them can look wildly different from one specialty to another. A surgeon might lean heavily on imaging and lab work, but a psychiatrist often has to navigate a world of overlapping symptoms where clear-cut objective tests are few and far between.
This is where the real art and flexibility of the diagnostic framework come into play. In fields like psychiatry, the "clues" aren't found in blood tests—they’re woven into a patient's life story, their behavior patterns, and their emotional state. The process shifts from pinpointing acute physical findings to building a rich, longitudinal history.
A Psychiatric Case Study: Bipolar vs. BPD
Think about the classic challenge of telling bipolar disorder apart from borderline personality disorder (BPD). At first glance, they can look remarkably similar. Both can show up with intense mood swings, impulsivity, and rocky relationships. A single snapshot of the patient in the ER can be incredibly misleading, which is why a thorough, long-term view is absolutely essential for an accurate differential.
To untangle them, a clinician has to dig much deeper:
Duration of Mood States: Bipolar disorder is defined by distinct episodes of mania or depression that last for days or even weeks. In stark contrast, the mood shifts in BPD are often rapid-fire, happening over the course of a few hours.
Triggers: The emotional rollercoaster in BPD is frequently a direct reaction to interpersonal stress, like a perceived slight or fear of abandonment. Bipolar mood episodes, on the other hand, tend to be more autonomous and less tied to specific external events.
Core Identity: Someone with bipolar disorder generally maintains a stable sense of self outside of mood episodes. A core feature of BPD, however, is a chronic disturbance in identity and persistent feelings of emptiness.
This kind of diagnostic detective work hinges on a structured, methodical approach. You can see just how vital this process is by looking at the evolution of psychiatric classification. The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) was a game-changer. The release of DSM-III in 1980, which introduced explicit diagnostic criteria, was a massive leap forward in making psychiatric diagnoses more reliable. You can learn more about the history of the DSM and its impact directly from the source.
This nuanced application proves that differential diagnosis isn't just a rigid formula. It’s a flexible way of thinking that adapts to the unique challenges of every medical field. It ensures that even when you don’t have a definitive lab test, you can still work methodically toward the most likely conclusion and, ultimately, provide the right care.
Frequently Asked Questions
Even with a solid framework, a few questions always pop up when you're first getting the hang of differential diagnosis. Let's tackle some of the most common ones to sharpen your understanding of this core clinical skill.
Think of this as firming up the foundation of your diagnostic thinking.
What Is the Difference Between a Differential and a Final Diagnosis?
A differential diagnosis is your opening gambit. It’s the structured list of all the possible culprits that could be causing a patient's signs and symptoms. This isn't just a random brainstorm; it's a working hypothesis that guides every test you order and every question you ask next.
A final diagnosis is where you land after all the detective work is done. It's the one confirmed condition left standing after you've methodically ruled everything else out from your initial list.
Simply put, the differential is the roadmap, and the final diagnosis is the destination.
How Does Clinical Experience Change the Diagnostic Process?
The way a clinician builds a differential diagnosis changes dramatically over time. Early on, new healthcare providers tend to create long, exhaustive lists. They work through every possibility to make sure nothing gets missed, which is a safe and necessary starting point.
But with years of practice, something shifts. Seasoned clinicians develop an almost intuitive sense of pattern recognition. They can look at a clinical picture and almost instantly narrow the possibilities down to the top three or four most likely causes. This leap, built on thousands of previous cases, is what allows them to get to the right answer faster and avoid a ton of unnecessary testing.
This skill becomes especially critical in fields like psychiatry, where symptoms can overlap across dozens of disorders. You can find more detail on the evolution of diagnostic methods on Wikipedia.
A working differential diagnosis is not just a list; it's a dynamic thought process. It reflects your current understanding of a patient's problem and is designed to change as new information comes to light.
How Do You Handle Cases With Multiple Conditions?
Real-world patients rarely present like clean textbook cases. More often than not, they're juggling multiple health issues at once, a situation we call comorbidity. This is where your differential diagnosis skills are truly put to the test.
When you suspect more than one thing is going on, your job is to untangle the clinical picture. You have to figure out which symptoms belong to which condition by systematically asking a few key questions:
- Could a single, underlying disease explain everything I'm seeing?
- Are these two completely separate problems that just happen to be occurring at the same time?
- Is one condition a complication or a direct result of another one?
For example, a patient with a long history of diabetes comes in with chest pain. Your differential has to weigh a cardiac cause (a known complication of diabetes) against something totally unrelated, like severe acid reflux. You have to treat each possibility as its own mini-investigation until you have a clear, complete picture of the patient's health.
Mastering the art of differential diagnosis is crucial for excelling on your board exams and becoming a confident clinician. At Ace Med Boards, we provide personalized, one-on-one tutoring to help you build the clinical reasoning skills you need to succeed. Our expert tutors guide you through high-yield topics and case-based questions for the USMLE, COMLEX, and Shelf exams.
Ready to sharpen your diagnostic skills? Schedule your free consultation with Ace Med Boards today!
