When you see the USMLE Step 3 average score—which generally sits around 228—it’s easy to breathe a sigh of relief if you’ve passed. And you should! But that number is more than just a passing benchmark; it’s a crucial piece of data for your career, especially if you have your sights set on competitive fellowships.
What Does the Step 3 Average Score Really Mean?
Think of the average score as the 50-yard line on a football field. Landing a 228 puts you squarely at the 50th percentile, meaning you performed better than half of the residents taking the exam. For most people grinding through their intern year, just getting a “pass” on the first try is a massive win, and rightfully so.
But the step 3 average score tells a bigger story. While your residency program director is likely just looking for that pass, fellowship directors in competitive fields often dig a little deeper.
Why the Average Matters for Ambitious Residents
A score that clears the average by a significant margin can be a real game-changer. It sends a clear signal to fellowship committees that you have a rock-solid clinical foundation and are ready for the next level of responsibility. This becomes particularly important in highly sought-after specialties like:
- Cardiology
- Gastroenterology
- Oncology
These fields are flooded with applications from incredibly qualified physicians. A high Step 3 score becomes a powerful tiebreaker, helping your file stand out from the stack. It shows you’re committed to going beyond the bare minimum.
A passing score keeps the door to residency open. An above-average score can unlock doors to the most competitive fellowships and career paths you might want down the road.
The average score for Step 3 has held steady around 228 for a while now. This reflects a test where most people do well enough to pass, but climbing into those upper percentiles takes a deliberate effort. You can learn more about the score distributions from the official Step 3 score distributions and pass rates data.
So, while you should absolutely celebrate passing, aiming to beat the average is a smart, strategic move. It's about building the strongest professional profile you can, right from the start of your residency.
Breaking Down Step 3 Scores and Percentiles
That three-digit score on your USMLE Step 3 report is more than just a number—it’s a direct reflection of how your clinical knowledge stacks up against thousands of your peers. To really get what it means, you have to look past the simple pass/fail line and understand where you land on the national performance curve.
The score itself runs on a scale from 1 to 300, and the magic number you need to hit is 200 to pass. While clearing that hurdle is obviously the main goal, your final score places you somewhere on a very wide spectrum of performance.
From Score to Percentile
Think of the scoring system like a leaderboard. The current average Step 3 score is around 228, which essentially splits the field right down the middle and lands you at the 50th percentile. In simple terms, a 228 means you performed better than half the residents who took the exam.
From there, every point you gain moves you up the ranks, signaling a stronger grasp of clinical knowledge. For instance, scoring a 240 pushes you into the top quarter of test-takers—a significant jump that can definitely get noticed by competitive fellowship programs. This chart gives you a quick visual breakdown of the general performance tiers.
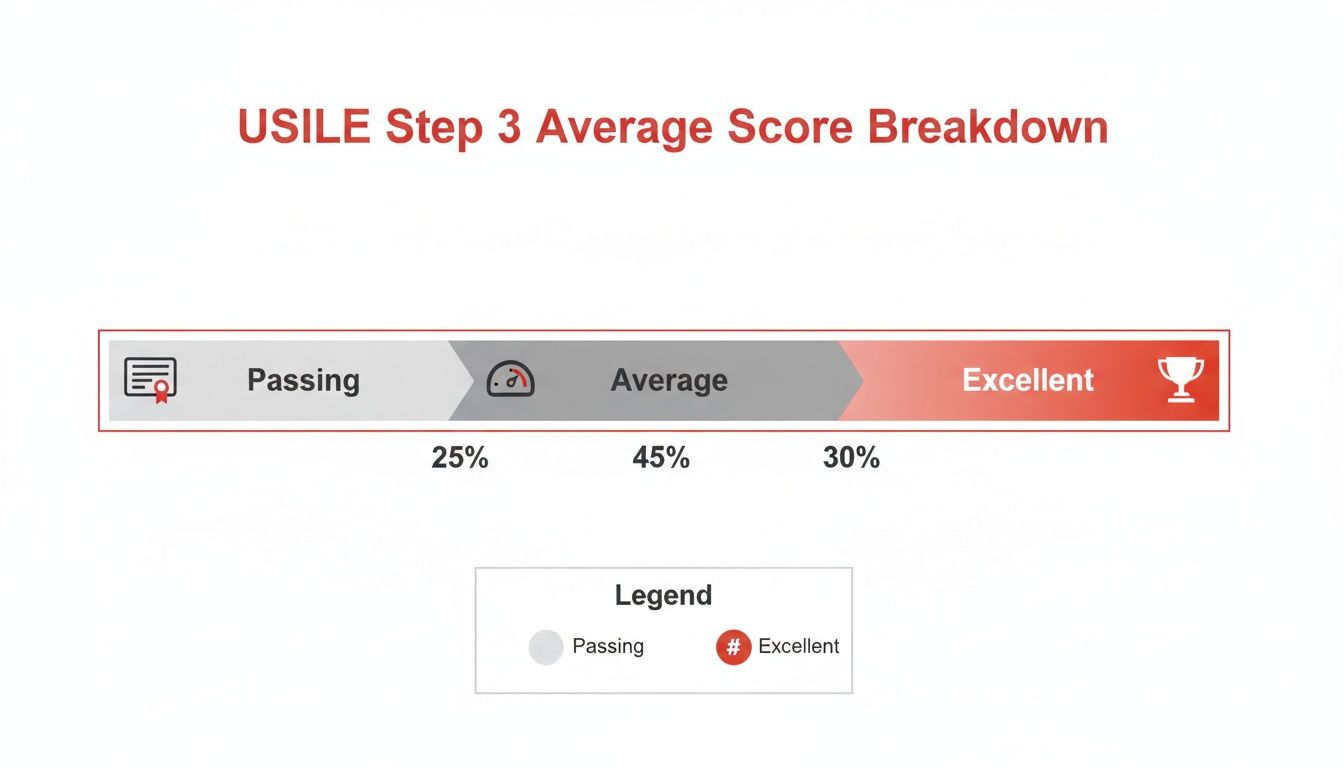
As you can see, just passing is the foundation. But a huge chunk of residents land in that average-to-excellent range, which is why a higher score can be such a powerful differentiator for your career.
Benchmarking Your Performance
Knowing where different scores fall is crucial for setting goals that are both realistic and ambitious. A score of 220, for example, is a comfortable pass but would likely place you just under the 50th percentile. On the flip side, a 240 launches you toward the 79th percentile, and any score cracking 250 marks you as a top-tier performer. For a deeper dive, you can always check out the official USMLE performance data.
Your Step 3 percentile isn't just for bragging rights; it's a strategic data point. It tells you how competitive you are for future opportunities and benchmarks your clinical skills against your national peer group.
To give you a clearer picture, here’s a table that provides an at-a-glance view of how different USMLE Step 3 scores correspond to estimated performance percentiles, helping you benchmark your target score.
USMLE Step 3 Score and Estimated Percentile Breakdown
| Score Range | Estimated Percentile | Performance Interpretation |
|---|---|---|
| 200-215 | 15th – 35th | Indicates a passing performance but falls below the national average. |
| 216-230 | 36th – 55th | Scores here are solidly average, showing competent clinical knowledge. |
| 231-245 | 56th – 80th | This is an above-average performance, signaling strong clinical skills. |
| 246+ | 81st+ | An excellent score that can significantly strengthen a fellowship application. |
Ultimately, translating your score into a percentile gives it context. It’s what turns an abstract number into a powerful tool for self-assessment and career planning, showing you exactly where you stand.
How Residency Programs View Your Step 3 Score
Once you get that Step 3 score report, it stops being just a personal milestone. It becomes a document that residency directors and, later on, fellowship committees will look at. While its importance can shift depending on who's looking, understanding their perspective is key to knowing just how much your performance matters.
For most residency program directors, your Step 3 score really only serves one purpose: a competency check. They just want to see a solid pass on the first attempt. This confirms you have the basic clinical judgment needed to practice medicine safely and effectively. A score right around the step 3 average score is perfectly fine and won't raise any red flags.
The Fellowship Application Game Changer
But the stakes change dramatically when you start thinking about competitive fellowships. If you’re aiming for fields like cardiology, gastroenterology, or demanding surgical subspecialties, that Step 3 score gets a major promotion. It transforms from a simple pass/fail metric into a powerful way to stand out.
For a residency program, a pass proves you can do the job. For a competitive fellowship, a high score is evidence you can excel in a high-pressure, specialized environment.
Think about it from their perspective. Program directors in these fields are drowning in applications from incredible candidates. When every applicant has glowing letters of recommendation and solid research, a Step 3 score of 245 or higher can be the thing that pulls your application out of the pile. It signals a depth of clinical knowledge that goes way beyond the minimum standard.
Special Considerations for IMGs
For International Medical Graduates (IMGs), the Step 3 score often carries even more weight. Program directors might use it as an extra data point to gauge your clinical readiness and how well you've adapted to the U.S. healthcare system. Nailing this exam with a score well above average can help quiet any potential concerns and make an IMG’s entire profile stronger.
- Demonstrates Clinical Acumen: A high score provides objective, undeniable proof of your clinical reasoning skills.
- Offsets Other Variables: It can help balance out other parts of an application that might be less competitive, like a lower Step 1 or Step 2 score.
- Shows Commitment: Performing well during the chaos of intern year shows incredible dedication and an ability to thrive under pressure.
Ultimately, your Step 3 score is just one piece of a much larger puzzle. To get a complete picture of what programs are looking for, our guide on the ERAS application process offers a deeper dive into building a well-rounded and competitive profile.
While a solid pass is enough for many, aiming to beat the step 3 average score is a strategic move, especially for anyone with ambitions for a top-tier fellowship. It’s an investment in your future, giving you a tangible metric of your expertise that can open doors to the next stage of your career. Your score becomes a part of your professional story.
Key Factors That Influence Step 3 Performance

Ever wonder why some residents seem to sail past the step 3 average score with ease while others just scrape by? It’s rarely just about raw medical knowledge. A few critical variables can make or break your performance, and understanding them is the first step toward building a study strategy that works with you, not against you.
One of the most noticeable and well-documented factors is the performance gap between U.S. medical graduates and International Medical Graduates (IMGs). This isn't a measure of capability, but rather a reflection of different training paths, clinical exposure, and even subtle language nuances in patient interactions.
The Graduate Background Divide
The data tells a clear story. Official USMLE pass rates for Step 3 show a tale of two different worlds. In 2023-2024, US/Canadian graduates had a near-perfect pass rate of 97%. In contrast, IMGs saw rates closer to 89-90%, a trend tracked across tens of thousands of test-takers annually.
So, where does this gap come from? It often boils down to differences in undergraduate medical education and hands-on clinical training. U.S. graduates are inherently more familiar with the exam’s specific format and the communication style expected in the patient simulations. For IMGs, closing this gap means making a conscious effort to adapt their clinical reasoning to the unique demands of the USMLE.
The Challenge of Timing and Balance
Another huge hurdle is simply when you take the exam during your intern year. Trying to study effectively while juggling 80-hour workweeks is a monumental task. The sheer exhaustion and stress of residency can take a direct toll on your cognitive function and your ability to retain new information.
The biggest battle for Step 3 isn't just mastering the content—it's mastering your schedule. Finding protected time to study consistently is often the difference between an average score and an exceptional one.
The timing within your PGY-1 year also plays a huge role:
- Early PGY-1: The foundational knowledge from med school is still fresh, which gives you a major leg up on the multiple-choice questions.
- Late PGY-1: You’ve got more real-world clinical experience under your belt, which can be priceless for the Computer-based Case Simulations (CCS).
There's no single "best" time to take it. It’s all about finding a window that aligns with the intensity of your residency schedule. A personalized plan is non-negotiable here. For a structured approach, our guide on crafting an effective Step 3 study plan provides a clear roadmap to navigate this challenge.
Finally, the quality of your study materials, especially question banks like UWorld, is a game-changer. But just having access isn't enough. Real success comes from using it to understand not just the what (the correct answer), but the why (the clinical logic behind it). This deliberate, active practice is what builds the skills needed to crush the average and get a score that truly reflects your potential.
Actionable Strategies to Exceed the Average Score

Knowing the step 3 average score is one thing, but actually beating it takes a smart, deliberate game plan. For residents with ambitious fellowship or career goals, just passing isn't enough. You need a practical, battle-tested playbook that fits into the chaos of residency.
The key is to focus your limited energy on the highest-impact areas. This isn’t just about what you study, but how you study. A winning approach means mastering high-yield multiple-choice topics while also becoming an expert on the Computer-based Case Simulations (CCS)—a section that regularly trips up even the sharpest residents.
Mastering the CCS Component
The CCS section is where many scores are made or broken. It’s not a simple test of knowledge; it’s about proving you can manage a patient systematically and competently. Think of it less like a traditional exam and more like a real clinical encounter that just happens to run on a clunky, outdated interface.
Success here boils down to two things: repetition and systemization. You need a consistent workflow for every single case, no matter the chief complaint. This ensures you never miss those critical, point-scoring actions.
- Initial Orders: Always start with the basics. Get vitals, pulse oximetry, IV access, and appropriate monitoring on every patient, every time.
- Systematic Workup: Move methodically from your history and physical to labs, imaging, and consults. Resist the urge to jump straight to a final diagnosis.
- Patient Disposition: Don't forget the easy points at the end. Move the patient to the right setting (like from the ED to an inpatient bed) and provide counseling on topics like smoking cessation or medication adherence.
Practicing with dedicated CCS software is completely non-negotiable. It builds the muscle memory you need to navigate the interface without thinking and reveals the specific management steps the USMLE rewards. Getting a feel for the exam style by reviewing sample USMLE Step 3 questions can also give you a major advantage for both the multiple-choice and case-based formats.
Building a Realistic Study Schedule
During Step 3 prep, your biggest enemy is the clock. A grueling residency schedule leaves almost zero room for error, making a realistic and flexible study plan absolutely essential. Forget cramming; consistency is what wins this race.
Aim for small, daily wins. One hour of focused study or completing two CCS cases per day is far more effective than trying to pull an all-nighter once a week.
Use techniques like spaced repetition to keep information fresh without having to constantly re-read everything. This means you review topics at increasing intervals, locking them into your long-term memory more efficiently. Be honest with yourself, identify your weak areas early, and dedicate a little extra time to them.
Beyond the books and software, your mental game is crucial. This is a marathon, not a sprint. Exploring strategies to improve mental stamina and resilience can make a huge difference in your ability to perform under pressure on exam day. These skills will help you turn all your hard work into an exceptional score that opens the right doors for your future.
Common Questions About the Step 3 Score
As you navigate the final stretch of your USMLE journey, it's natural for questions to pop up. With the step 3 average score as a common benchmark, most residents are trying to figure out how to best position themselves for success while juggling the insane demands of intern year. Let's tackle some of the most pressing questions head-on.
When Is the Best Time to Take Step 3?
Most residents opt to take Step 3 during their intern year (PGY-1), and for good reason. Your foundational clinical knowledge is still fresh, which is a huge help for the Foundations of Independent Practice (FIP) questions that cover more general medicine.
However, there's a strong case for waiting until late in your PGY-1 year or even early PGY-2. By then, you'll have much more hands-on clinical experience under your belt. This real-world practice is a massive advantage for the Advanced Clinical Medicine (ACM) and, especially, the Computer-based Case Simulations (CCS) parts of the exam. Ultimately, the perfect time hinges on your personal study rhythm and the realities of your residency schedule.
Is Failing Step 3 a Major Red Flag?
Let's be clear: passing on your first attempt is what everyone aims for. But a single failure isn't a career-ender, as long as you can bounce back and pass comfortably the next time. You just have to be ready to own it and honestly discuss what you learned from the experience in future fellowship interviews.
A failed attempt is a setback, not a stop sign. The key is to address your weak areas decisively, prove your resilience, and come back stronger on your retake.
That said, for highly competitive fellowships, a failure on your record can be a significant hurdle. It really underscores how important it is to be fully prepared the first time you walk into that testing center to keep all your future career doors wide open.
How Important Is the CCS Section?
The Computer-based Case Simulations (CCS) are critically important—don't let anyone tell you otherwise. This section makes up a huge chunk of your final score and is designed to directly test your real-time clinical management skills, not just what you've memorized.
Many otherwise strong test-takers make the mistake of underestimating the CCS portion, and they often see their scores suffer for it. A great performance on the cases can pull a borderline score up significantly, while a poor one can easily tank an excellent multiple-choice performance. Dedicated practice with CCS software isn't just a suggestion; it's absolutely non-negotiable if you're aiming for a high score.
Ready to build a strategy that pushes you past the average and prepares you for every section of the exam? Ace Med Boards offers personalized, one-on-one tutoring designed to fit your unique needs and busy residency schedule. Learn more and book a free consultation at https://acemedboards.com.
