The USMLE Step 2 CK isn't just a test of knowledge; it's a rigorous assessment of clinical reasoning, pattern recognition, and decision-making under pressure. Simply memorizing facts from a textbook is an insufficient strategy for success. To excel, you must learn to think like a seasoned clinician, dissecting each question stem for critical clues and navigating through complex differential diagnoses to arrive at the single best answer. This requires a specific mindset that goes far beyond rote learning.
This guide is designed to help you cultivate that mindset. We will break down eight classic, high-yield scenarios that mirror what you'll encounter on exam day. We won't just give you the answers; we'll deconstruct a curated set of Step 2 CK sample questions to reveal the underlying strategy behind them. You'll learn how to identify the “money” words, weigh competing options, and apply key concepts efficiently and accurately.
While mastering clinical knowledge is paramount, developing strong interpersonal and effective communication skills is also vital for understanding patient presentations, a key aspect of clinical reasoning. Our goal is to transform your approach from passive learning to active problem-solving, equipping you with the tactical skills needed for a top score. Let’s begin.
1. Acute Chest Pain with ECG Changes
One of the most critical scenarios you'll encounter in step 2 ck sample questions is the patient presenting with acute chest pain, a classic sign of potential myocardial infarction (MI). This question type tests your ability to rapidly interpret an electrocardiogram (ECG), identify the type of MI, and initiate the correct management protocol under time pressure. The vignette of a 55-year-old male with chest pain radiating to his left arm and ST-elevation in leads II, III, and aVF is a textbook presentation of an inferior wall ST-elevation myocardial infarction (STEMI).
Strategic Analysis
The core challenge is not just diagnosis but immediate, life-saving intervention. The USMLE will expect you to know the management algorithm for STEMI, which prioritizes timely reperfusion to salvage myocardial tissue. Your decision between primary percutaneous coronary intervention (PCI) and thrombolytic therapy is paramount and depends heavily on logistical factors like hospital capabilities and transfer times.
Actionable Takeaways & Tips
To master these questions, focus on a systematic approach:
- ECG Mastery: Memorize which ECG leads correspond to which coronary artery territories (e.g., II, III, aVF for the right coronary artery).
- Time is Myocardium: Understand the critical time goals. The target for "door-to-balloon" time for PCI is 90 minutes. If a patient is at a non-PCI-capable hospital, the total time from first medical contact to device deployment should be within 120 minutes.
- Thrombolytic Contraindications: Know the absolute contraindications to thrombolytics, such as a history of hemorrhagic stroke, recent ischemic stroke, or active internal bleeding.
This decision tree infographic outlines the critical management pathway for a patient with a suspected inferior STEMI.
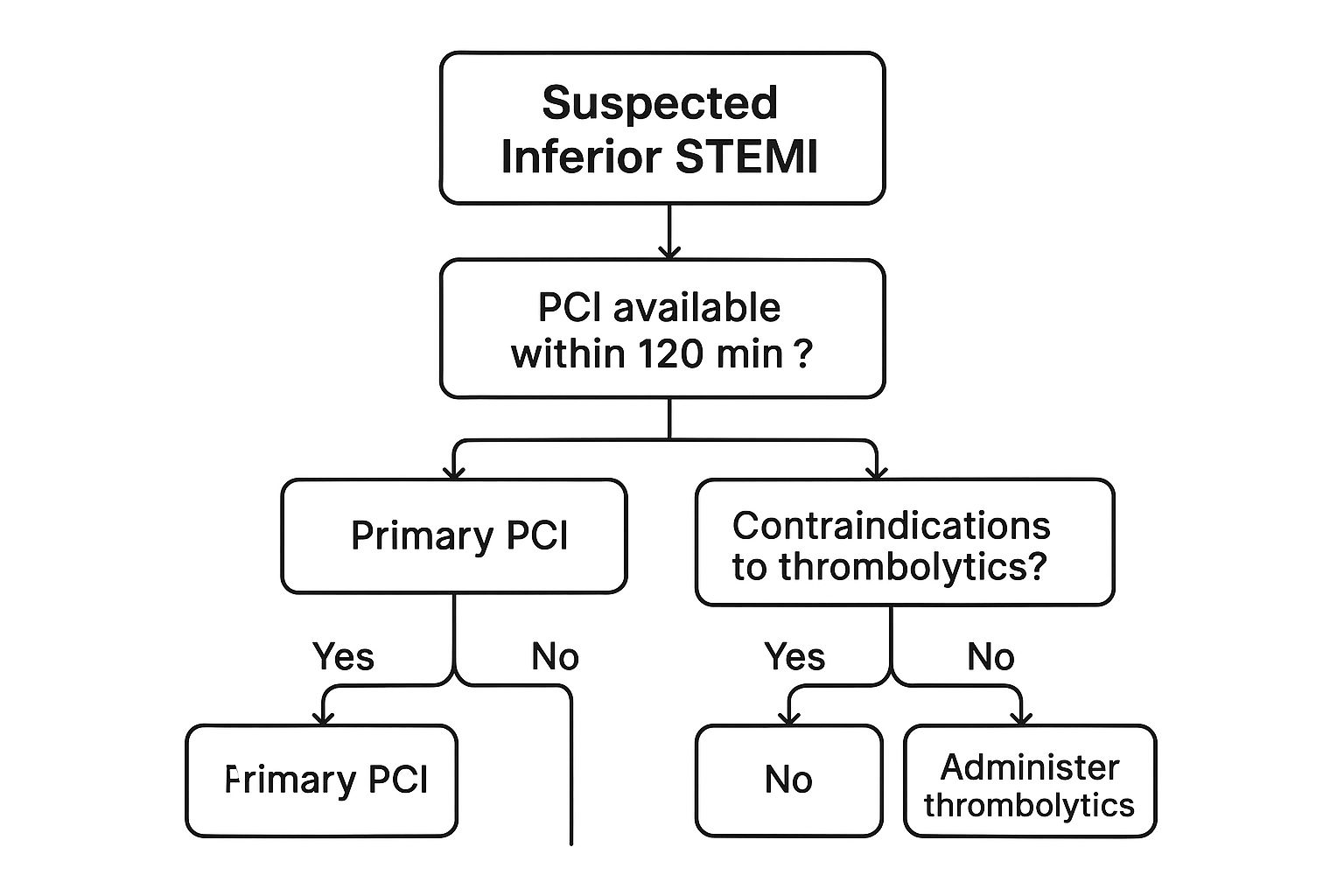
The infographic clearly illustrates that the primary decision point is whether PCI can be performed within 120 minutes, guiding the choice between immediate intervention, thrombolysis, or transfer. For more in-depth strategies on tackling high-yield clinical scenarios, check out this guide on how to study for Step 2 CK.
2. Pediatric Fever and Rash Presentation
A classic pediatric vignette you will encounter in step 2 ck sample questions involves a young child with a prolonged fever and a distinct constellation of symptoms. The presentation of a 4-year-old with a 5-day high fever, bilateral non-exudative conjunctivitis, a "strawberry tongue," and a polymorphous rash is a textbook case of Kawasaki disease. This question type assesses your ability to recognize this acute vasculitis and, more importantly, to initiate treatment promptly to prevent severe long-term cardiac complications.

Strategic Analysis
The challenge here lies in differentiating Kawasaki disease from other common childhood febrile illnesses and understanding the urgency of treatment. The USMLE will test your knowledge of the diagnostic criteria and the critical management step: administering intravenous immunoglobulin (IVIG) and high-dose aspirin. The primary goal of this therapy is to reduce the systemic inflammation that can lead to coronary artery aneurysms, the most feared complication of the disease.
Actionable Takeaways & Tips
To excel on these pediatric questions, focus on the diagnostic framework and treatment protocol:
- Memorize the "CRASH and Burn" mnemonic: This helps recall the criteria: Conjunctivitis, Rash, Adenopathy (cervical), Strawberry tongue (and other mucosal changes), and Hand/foot changes (edema/erythema), plus a Burn (fever for at least 5 days).
- Prioritize Immediate Treatment: Know that IVIG and high-dose aspirin are the first-line treatments. The question will hinge on you selecting this combination over antibiotics or expectant management.
- Focus on the Complication: Always associate Kawasaki disease with the risk of coronary artery aneurysms. This understanding frames the entire management strategy and follow-up, which includes echocardiography.
The key to this scenario is recognizing a specific pattern and knowing the non-negotiable first-line therapy. To further solidify your knowledge of high-yield pediatric topics for your shelf exams, explore our targeted Pediatrics shelf exam tutoring.
3. Altered Mental Status in Elderly Patient
A frequent high-yield scenario found in step 2 ck sample questions involves an elderly patient with a sudden change in mental status. These questions challenge your ability to look beyond the obvious presenting complaint and consider a broad differential diagnosis. A classic vignette describes an 82-year-old nursing home resident brought in for acute confusion, who also has a fever, tachycardia, and hypotension, suggesting sepsis likely originating from a urinary tract infection (UTI). This tests your understanding of atypical presentations of severe infections in the geriatric population.
Strategic Analysis
The primary challenge in this scenario is recognizing that altered mental status in an elderly patient is often the first, and sometimes only, sign of a serious underlying medical condition like an infection. The USMLE expects you to connect subtle clues such as dysuria with systemic signs of sepsis and initiate aggressive management promptly. Your ability to apply sepsis criteria like SIRS or qSOFA to an atypical presentation is crucial for a high score on these questions.
Actionable Takeaways & Tips
To excel at these questions, adopt a systematic approach for elderly patients with confusion:
- Atypical is Typical: Remember that classic signs of infection like fever and localized pain may be absent in the elderly. Delirium or functional decline can be the sole manifestation of a severe illness.
- Sepsis Screening: Be quick to apply scoring systems like the qSOFA score (respiratory rate ≥22/min, altered mentation, systolic BP ≤100 mm Hg). A score of 2 or more indicates a high risk for poor outcomes in patients with suspected infection.
- Broaden the Differential: While UTI is a common cause, always consider other sources of infection like pneumonia, as well as non-infectious causes like medication side effects, metabolic disturbances, or stroke.
- Empiric Antibiotics: Know the appropriate empiric antibiotic coverage for a suspected UTI leading to sepsis, often involving a broad-spectrum agent like a third-generation cephalosporin or piperacillin-tazobactam.
4. Pregnant Patient with Hypertension
A frequently tested and high-stakes topic in step 2 ck sample questions involves the pregnant patient presenting with hypertension. This scenario requires you to differentiate among hypertensive disorders of pregnancy and initiate urgent management to prevent life-threatening complications for both mother and fetus. A classic vignette describes a woman in her third trimester with a severe-range blood pressure, headache, and lab abnormalities, pointing toward preeclampsia with severe features.
Strategic Analysis
The critical task in these questions is to recognize the signs of severe disease and act decisively. The USMLE will test your ability to diagnose preeclampsia with severe features and immediately implement the correct treatment protocol. This includes initiating seizure prophylaxis with magnesium sulfate and controlling dangerously high blood pressure, all while understanding that definitive treatment is delivery of the fetus and placenta.
Actionable Takeaways & Tips
To excel in these high-pressure obstetrics questions, a structured approach is key:
- Know the Criteria: Memorize the diagnostic criteria for preeclampsia with severe features, including systolic BP ≥ 160 mm Hg or diastolic BP ≥ 110 mm Hg, thrombocytopenia, elevated liver enzymes, severe right upper quadrant pain, progressive renal insufficiency, pulmonary edema, or new-onset visual disturbances.
- Master Magnesium: Understand the role of magnesium sulfate for seizure prophylaxis. Know the signs of toxicity (e.g., loss of deep tendon reflexes, respiratory depression) and the antidote (calcium gluconate).
- Hypertensive Urgency: Be familiar with the first-line intravenous antihypertensives safe in pregnancy, such as labetalol, hydralazine, and nifedipine.
- Definitive Treatment: Remember that delivery is the ultimate cure for preeclampsia. For a patient at or beyond 34 weeks gestation with severe features, prompt delivery is indicated.
5. Diabetic Patient with Abdominal Pain
A cornerstone of endocrinology questions in step 2 ck sample questions involves a patient with known diabetes presenting with a severe metabolic disturbance. This scenario tests your ability to recognize and manage diabetic ketoacidosis (DKA), a life-threatening complication. The vignette of a 45-year-old with Type 1 diabetes, abdominal pain, a blood glucose of 450 mg/dL, and an anion gap metabolic acidosis (pH 7.25 with positive ketones) is a classic presentation of DKA, often triggered by an underlying infection or non-compliance with insulin.
Strategic Analysis
The primary challenge in this question is not just diagnosing DKA but executing the multi-step management protocol in the correct sequence. The USMLE will test your understanding of fluid resuscitation, insulin administration, and electrolyte monitoring and replacement. A common pitfall is giving insulin without first addressing the patient's volume status and potassium level, which can lead to life-threatening hypokalemia and cardiovascular collapse.
Actionable Takeaways & Tips
To confidently manage DKA scenarios, commit these steps to memory:
- Diagnose with the Triad: Solidify your understanding of the diagnostic criteria for DKA: hyperglycemia (glucose >250 mg/dL), ketonemia/ketonuria, and an anion gap metabolic acidosis (pH <7.3, bicarbonate <18 mEq/L).
- Fluids First: The initial and most critical step is aggressive intravenous fluid resuscitation with normal saline. This restores intravascular volume, improves renal perfusion, and helps lower blood glucose.
- Potassium is Key: Before starting an insulin drip, always check the serum potassium. Insulin drives potassium into cells, so you must ensure the level is >3.3 mEq/L to prevent severe hypokalemia. Replete potassium if necessary.
- Insulin and Dextrose Protocol: Once fluids and potassium are addressed, begin a continuous IV insulin infusion. When the patient's blood glucose falls to around 200-250 mg/dL, add dextrose (D5) to the IV fluids to prevent hypoglycemia while you continue to correct the acidosis and close the anion gap.
Mastering DKA management is a high-yield topic that frequently appears in both Step 2 and internal medicine shelf exams. To dive deeper into these core clinical topics, explore this comprehensive internal medicine shelf review.
6. Young Adult with Shortness of Breath
A frequent clinical scenario presented in step 2 ck sample questions is the young, otherwise healthy patient who develops sudden-onset dyspnea and pleuritic chest pain. This classic vignette, often featuring a tall, thin male, is designed to test your recognition and management of a primary spontaneous pneumothorax (PSP). A typical question will describe a 25-year-old male with these symptoms and include a chest X-ray finding of absent lung markings, pointing directly to the diagnosis.
Strategic Analysis
The core of this question type revolves around management decisions based on the size of the pneumothorax and the patient's clinical stability. The USMLE will challenge you to differentiate between a stable patient who can be observed and an unstable patient requiring immediate intervention. Knowing the specific criteria for intervention, such as hemodynamic instability or a large pneumothorax (typically >3 cm from the chest wall at the apex), is crucial for selecting the correct answer.
Actionable Takeaways & Tips
To confidently answer these questions, your preparation should focus on the management algorithm for PSP:
- Size Matters: Learn how to quickly assess pneumothorax size on imaging. A small pneumothorax (<3 cm apex-to-cupola distance) in a stable patient is often managed with observation and supplemental oxygen.
- Intervention Thresholds: Understand the clear indications for intervention. A large pneumothorax or any pneumothorax in a clinically unstable patient (e.g., hypotensive, hypoxic) requires needle decompression or chest tube (thoracostomy) placement.
- Know the Demographics: Remember the classic risk factor profile. Tall, thin males, smokers, and individuals with a family history or underlying Marfan syndrome are at the highest risk for primary spontaneous pneumothorax.
- Recurrence and Prevention: Be aware of the next steps for recurrent pneumothorax. These cases often require surgical intervention, such as video-assisted thoracoscopic surgery (VATS) with pleurodesis, to prevent future episodes.
7. Mental Health Crisis in Emergency Setting
A frequent and high-stakes scenario in step 2 ck sample questions involves a patient presenting to the emergency department (ED) with an acute psychiatric crisis. The vignette of a 19-year-old college student with active suicidal ideation, a specific plan, and recent behavioral changes (giving away belongings) is a classic setup. This question type tests your ability to rapidly assess suicide risk, initiate immediate safety protocols, and navigate the complex legal and ethical duties of a physician in a psychiatric emergency.
Strategic Analysis
The core challenge is balancing patient autonomy with the duty to protect the patient from harm. The USMLE will expect you to recognize that a patient with a clear plan, intent, and means for suicide lacks the capacity to make decisions about their own safety. Your primary responsibility is to prevent self-harm, which often requires involuntary intervention. The decision to admit a patient to an inpatient psychiatric unit, even against their will, is a critical step based on a thorough risk assessment.
Actionable Takeaways & Tips
To confidently answer these questions, your approach must be systematic and legally sound:
- Standardized Risk Assessment: Familiarize yourself with key components of a suicide risk assessment. Always ask directly about plan, intent, means, and access to those means. The presence of all these factors indicates a very high-risk patient.
- Involuntary Holds: Understand the criteria for an involuntary psychiatric hold (often called a "72-hour hold" or similar, depending on jurisdiction). A patient is typically eligible if they are a danger to themselves, a danger to others, or gravely disabled.
- Prioritize Safety: In any psychiatric emergency involving potential harm, the first step is to ensure the safety of the patient and staff. This may involve one-to-one observation or removing dangerous objects from the patient's vicinity.
- Early Consultation: Know that the correct next step after ensuring immediate safety is often to obtain an urgent psychiatric consultation. This demonstrates a collaborative and appropriate approach to management.
8. Infectious Disease with Travel History
A common and high-yield scenario in step 2 ck sample questions involves a patient presenting with systemic symptoms after recent international travel. These questions assess your ability to connect clinical findings with epidemiological risk factors. A classic vignette might describe a 35-year-old who develops fever, chills, and headaches 10 days after returning from a trip to Sub-Saharan Africa, with a blood smear revealing intraerythrocytic parasites, a textbook presentation of malaria.
Strategic Analysis
The critical skill tested here is formulating a differential diagnosis based on geographic exposure. The USMLE will expect you to recognize key infectious diseases endemic to specific regions and initiate the appropriate diagnostic workup and treatment. For a malaria case, this includes identifying the most likely Plasmodium species based on travel location and knowing the corresponding first-line treatments, which vary significantly due to regional drug resistance.
Actionable Takeaways & Tips
To excel in these travel medicine questions, integrate the following strategies into your preparation:
- Geographic Associations: Create a "bug-to-drug-by-region" map. For instance, associate chloroquine-resistant P. falciparum with Sub-Saharan Africa and Southeast Asia, and know that primaquine is needed for the dormant liver stages of P. vivax and P. ovale.
- Detailed History is Key: Always pay close attention to the travel history provided in the vignette, including the timing of symptom onset relative to travel, specific activities (e.g., freshwater swimming, insect bites), and prophylaxis use.
- Know the Classics: Memorize the classic presentations of high-yield travel-related illnesses: malaria (cyclical fevers), dengue (fever, retro-orbital pain, rash, thrombocytopenia), typhoid fever (fever, relative bradycardia, rose spots), and schistosomiasis (portal hypertension, eosinophilia).
- Treatment Protocols: Understand the first-line treatments for uncomplicated versus severe malaria. For example, atovaquone-proguanil or artemether-lumefantrine for uncomplicated falciparum malaria, and intravenous artesunate for severe cases.
Step 2 CK Sample Question Scenarios Comparison
| Condition | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Acute Chest Pain with ECG Changes | Moderate – requires ECG interpretation and decision-making under pressure | High – ECG, catheterization lab, reperfusion therapy | High impact – timely reperfusion reduces mortality | Emergency medicine, STEMI recognition and management | Clear ECG criteria, high-yield emergency topic |
| Pediatric Fever and Rash Presentation | Moderate – understanding specific diagnostic criteria | Moderate – clinical exam, IVIG treatment resources | Prevents serious cardiac complications like aneurysms | Pediatric emergency and cardiology settings | Clear criteria, integrates multispecialty knowledge |
| Altered Mental Status in Elderly Patient | High – requires recognition of atypical presentations and differential diagnosis | Moderate – labs, imaging, antibiotic access | Improves mortality by early sepsis recognition and treatment | Geriatrics, emergency, infectious disease | Common scenario, emphasizes early recognition |
| Pregnant Patient with Hypertension | Moderate to high – multiple parameters and maternal-fetal considerations | High – labs, maternal-fetal monitoring, medication safety | Reduces maternal and fetal morbidity and mortality | Obstetric emergencies, hypertensive disorders | Well-established protocols, multi-specialty relevance |
| Diabetic Patient with Abdominal Pain | Moderate – needs acid-base and insulin management knowledge | Moderate to high – labs, ICU care, insulin administration | Effective DKA management reduces mortality and complications | Emergency and endocrinology settings | Standardized protocols, integrates physiology |
| Young Adult with Shortness of Breath | Low to moderate – requires chest X-ray interpretation and procedural skills | Moderate – imaging, chest tube placement availability | Rapid symptom relief, complication prevention | Pulmonary emergencies, trauma care | Clear imaging findings, straightforward algorithms |
| Mental Health Crisis in Emergency Setting | High – subjective assessment, legal complexity | Low to moderate – psychiatric resources and legal frameworks | Prevents suicide, ensures patient safety and legal compliance | Psychiatric emergencies, general medical care | Standardized tools, crucial for all specialties |
| Infectious Disease with Travel History | Moderate – requires travel history and parasitology understanding | Moderate – lab testing, antimalarials, infectious disease consultation | Early diagnosis prevents fatal outcomes | Travel and tropical medicine, infectious disease | Clear diagnostics, critical for global health |
Turn Your Knowledge into a Winning Score
Navigating the USMLE Step 2 CK exam is less about memorizing every obscure fact and more about mastering the art of clinical reasoning under pressure. The step 2 ck sample questions we've dissected throughout this article are not just isolated scenarios; they are blueprints for the types of high-stakes decisions you will be expected to make. Each question, from the acute MI workup to the nuanced management of a psychiatric emergency, serves as a masterclass in pattern recognition and strategic thinking.
The core lesson is this: success hinges on your ability to rapidly identify the "ill vs. not ill" patient, formulate a prioritized differential diagnosis, and select the single most appropriate next step. It’s a process that demands both deep medical knowledge and a structured, systematic approach to problem-solving. By internalizing these frameworks, you transform your study sessions from passive review into active, exam-specific training.
Key Strategic Takeaways for Your Preparation
As you move forward, keep these core principles at the forefront of your study plan. They represent the bridge between knowing the information and applying it effectively on exam day.
- Master the "Next Best Step" Mindset: For every clinical vignette, your primary goal is to determine the immediate priority. Is it stabilizing the patient (ABCs), confirming a diagnosis, or initiating treatment? This hierarchical thinking is critical, as seen in our acute chest pain and altered mental status examples.
- Recognize Classic Illness Scripts: The Step 2 CK is built on archetypal presentations. The febrile child with a specific rash, the pregnant patient with elevated blood pressure, or the traveler with an unusual infection are classic "illness scripts." Learning to spot these patterns quickly saves valuable time and mental energy.
- Integrate Risk Factors and Demographics: Always consider the patient's age, comorbidities, and social history (like travel or substance use). These details are never random; they are crucial clues designed to guide you toward the correct diagnosis, as demonstrated in the elderly patient with delirium and the diabetic patient with abdominal pain.
- Don't Just Memorize, Understand: Instead of just memorizing that preeclampsia requires magnesium sulfate, understand why it's the first-line therapy for seizure prophylaxis. This deeper level of comprehension allows you to apply principles to atypical presentations and answer second or third-order questions with confidence.
Ultimately, your performance on the Step 2 CK is a direct reflection of your ability to think like a competent, confident resident. The sample questions and strategies provided here are designed to build that exact skillset. Treat every practice question as a clinical encounter. Analyze the data, weigh the options, and commit to a decision. This deliberate practice is what forges exceptional clinicians and leads to top-tier scores.
Ready to elevate your preparation from good to great? The expert tutors at Ace Med Boards specialize in transforming your understanding of complex topics into high scores by helping you master the strategic approach to step 2 ck sample questions and beyond. Visit Ace Med Boards to learn how personalized guidance can unlock your full potential and help you achieve your target score.
