The USMLE Step 3 exam marks a critical transition from theoretical knowledge to practical clinical application. Unlike previous steps that heavily test foundational science, Step 3 focuses on your ability to function as an unsupervised physician, managing patients in ambulatory and inpatient settings. It’s not just about what you know; it’s about what you can do with that knowledge under pressure. This listicle moves beyond simple rote memorization to provide a curated set of sample USMLE Step 3 questions that mirror the complexity of the real exam.
Each example is designed to sharpen your clinical reasoning skills. We will dissect high-yield cases, from managing an acute coronary syndrome to assessing a psychiatric emergency, providing a detailed breakdown of the correct answer and, more importantly, the strategic thinking required to arrive at it. You will learn to identify key diagnostic clues, select appropriate next steps, and avoid common pitfalls. To move 'Beyond Memorization' and truly master USMLE Step 3 clinical cases, leveraging interactive tools like the tnote.ai editor can help you create, refine, and organize your own study materials and case notes. This guide offers actionable takeaways to help you think like a senior resident and confidently tackle both the multiple-choice questions and the challenging Computer-based Case Simulations (CCS).
1. Acute Coronary Syndrome Management
Acute Coronary Syndrome (ACS) is a high-yield, high-stakes topic on the USMLE Step 3. Questions on this subject test your ability to quickly interpret clinical data, such as ECGs and cardiac biomarkers, and initiate time-sensitive management protocols. These scenarios often involve complex patient presentations and require you to make critical decisions under pressure, mirroring real-world clinical practice. Understanding ACS is fundamental because it directly assesses your readiness for unsupervised medical practice.
A typical sample USMLE Step 3 question might feature a 65-year-old male with crushing chest pain and ST-segment elevations in leads II, III, and aVF (inferior wall STEMI). You would need to immediately recognize the need for reperfusion therapy. Another variation could involve a diabetic patient with only vague epigastric discomfort and fatigue but significantly elevated troponins, forcing you to diagnose an NSTEMI and decide on the timing for cardiac catheterization.
Strategic Approach and Key Takeaways
Success with ACS questions hinges on a systematic approach to diagnosis and risk stratification. You must rapidly differentiate between unstable angina, NSTEMI, and STEMI, as the management pathways diverge significantly.
- Initial Triage: Always start with an ECG within 10 minutes and check cardiac troponins. The ECG is the most critical initial diagnostic tool.
- STEMI Protocol: For ST-segment elevation MI, the mantra is "time is muscle." Your immediate goal is reperfusion. Remember the door-to-balloon time of less than 90 minutes for PCI or, if unavailable, fibrinolysis within 30 minutes.
- NSTEMI/UA Protocol: For non-ST-segment elevation ACS, risk stratification using TIMI or GRACE scores is key. This helps determine whether an early invasive strategy (cardiac cath within 24 hours) or a conservative approach is more appropriate.
Test-Taking Tip: Be vigilant for contraindications. Before selecting an answer involving anticoagulants like heparin or fibrinolytics like alteplase, always scan the patient vignette for any history of recent major bleeding, stroke, or surgery.
The following infographic illustrates the core decision-making process for managing a patient presenting with suspected ACS.
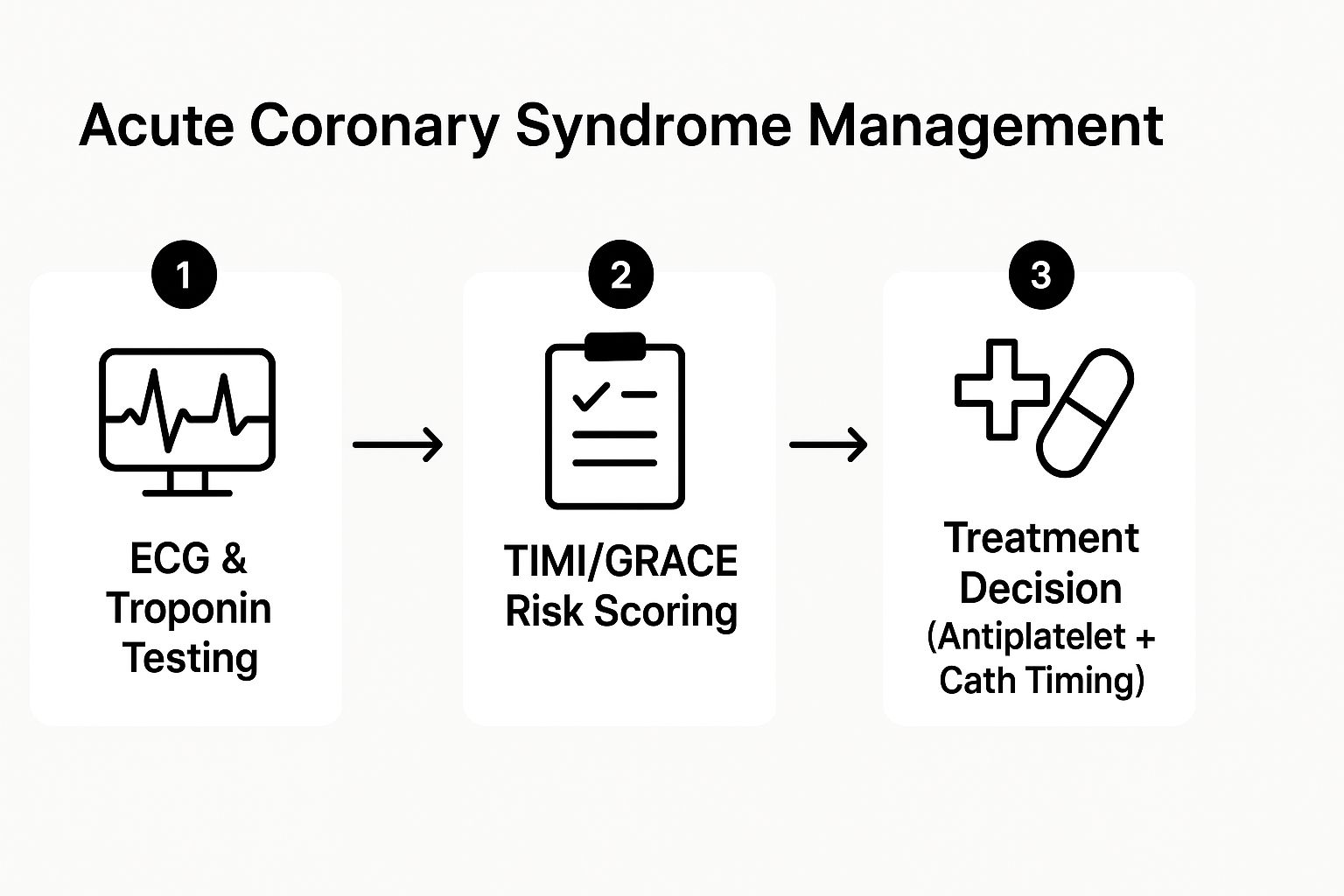
This workflow emphasizes that after initial testing, risk scoring is the critical pivot point that dictates the urgency and type of intervention.
Mastering these pathways is not just about memorization; it's about applying clinical reasoning. For more in-depth study strategies, you can explore additional medical school exam preparation tips.
2. Pediatric Febrile Seizure Management
Pediatric febrile seizures are a common and often frightening presentation in the emergency department, making them a high-yield topic for the USMLE Step 3. Questions in this domain assess your ability to differentiate benign, simple febrile seizures from more complex cases that may signal a serious underlying infection like meningitis. The exam tests your clinical judgment in determining the necessary workup, providing appropriate acute management, and effectively counseling anxious parents, which are core competencies for an independent physician.
A classic sample USMLE Step 3 question might describe an 18-month-old child who experienced a single, generalized tonic-clonic seizure lasting three minutes during a febrile illness. The child is now postictal but arousable. You would need to identify this as a simple febrile seizure and choose reassurance and antipyretics as the next step. A more complex variant could involve a 9-month-old with an incomplete immunization history presenting with a focal seizure or multiple seizures in 24 hours, requiring you to consider a lumbar puncture to rule out meningitis.
Strategic Approach and Key Takeaways
Success with febrile seizure questions requires a firm grasp of diagnostic criteria and American Academy of Pediatrics (AAP) guidelines. The key is to quickly classify the seizure and identify any red flags that warrant a more extensive investigation beyond supportive care.
- Differentiate Simple vs. Complex: This is the most critical first step. A simple febrile seizure is generalized, lasts <15 minutes, and does not recur within 24 hours. Any deviation (focal features, duration >15 minutes, or recurrence) classifies it as complex and lowers the threshold for further workup.
- Know Lumbar Puncture (LP) Indications: The AAP strongly recommends an LP for any child with a febrile seizure who has meningeal signs. An LP should be considered for infants 6-12 months old with incomplete or unknown immunization status for H. influenzae type b or S. pneumoniae. It is also an option for children who are on antibiotics, as treatment can mask meningeal signs.
- Focus on the Fever Source: After stabilizing the patient, the management priority shifts to identifying and treating the cause of the fever (e.g., otitis media, pharyngitis, or urinary tract infection).
Test-Taking Tip: Questions often focus on parental counseling. Be prepared to choose the answer that accurately communicates the benign nature of simple febrile seizures, the lack of association with long-term epilepsy, and the approximate 30-40% risk of recurrence. Reassurance is a key management step.
The primary goal is to ensure no serious underlying pathology is missed while avoiding unnecessary, invasive procedures in a child with a benign condition. Mastering this balance is essential for both the exam and clinical practice. For more guidance on tackling challenging clinical scenarios, you can find valuable resources on USMLE Step 3 preparation strategies.
3. Diabetes Mellitus Complications and Management
Diabetes Mellitus (DM) is a cornerstone of primary care and a frequently tested topic on the USMLE Step 3. Questions go beyond simple diagnosis, focusing on the management of both acute crises and chronic sequelae. These scenarios test your ability to synthesize patient history, lab data, and physical exam findings to initiate appropriate therapy and adjust long-term care plans, reflecting the responsibilities of a general practitioner.
A classic sample USMLE Step 3 question could present a young patient with rapid breathing, fruity-scented breath, and altered mental status, requiring you to diagnose Diabetic Ketoacidosis (DKA) and immediately initiate an insulin drip and fluid resuscitation. Another common scenario might involve an elderly patient with Type 2 diabetes presenting with profound dehydration and confusion, pointing towards a Hyperosmolar Hyperglycemic State (HHS). You must differentiate these emergencies and manage them according to established protocols.
Strategic Approach and Key Takeaways
Success with DM questions requires a firm grasp of both emergency protocols and outpatient management guidelines. You must be able to recognize a diabetic emergency, stabilize the patient, and then transition to long-term care planning.
- Emergency Management: For DKA and HHS, the priorities are IV fluids, insulin administration, and careful electrolyte monitoring, especially potassium. Remember to correct potassium before starting insulin if it's low.
- Chronic Complication Screening: Know the American Diabetes Association (ADA) guidelines. This includes annual screening for nephropathy (urine albumin-to-creatinine ratio), retinopathy (dilated eye exam), and neuropathy (monofilament test).
- Pharmacologic Nuances: Understand the mechanisms and major side effects of different drug classes. For instance, recognize that SGLT2 inhibitors (e.g., empagliflozin) offer cardiovascular benefits but are contraindicated in patients with a low GFR and can increase the risk of euglycemic DKA.
Test-Taking Tip: When a patient with diabetes presents with altered mental status, diabetic emergencies like DKA, HHS, or severe hypoglycemia should be at the top of your differential diagnosis. Always check a fingerstick glucose early in the workup.
The management of diabetes is a dynamic process. It involves treating the immediate problem while simultaneously considering the long-term implications for the patient's health. For more practice, you can work through additional sample USMLE questions.
4. Psychiatric Emergency Assessment
Psychiatric emergencies are a critical component of the USMLE Step 3, as they test your ability to manage high-risk situations that require immediate, decisive action. These questions assess your skills in rapidly evaluating safety, differentiating psychiatric from medical etiologies, and understanding the legal and ethical framework for involuntary treatment. Proficiency in this area is essential for any physician, as these presentations can occur in any clinical setting, from the emergency department to a primary care clinic.
A typical sample USMLE Step 3 question might present a 22-year-old college student brought in by roommates for paranoid delusions and auditory hallucinations (a first-episode psychosis). You would need to rule out substance-induced psychosis or underlying medical conditions before initiating antipsychotic medication and determining the need for hospitalization. Another common scenario involves a patient with known major depressive disorder who expresses active suicidal ideation with a plan, requiring you to assess the level of risk and initiate involuntary commitment procedures.
Strategic Approach and Key Takeaways
Your success with psychiatric emergency questions depends on a structured and safety-oriented approach. The primary goal is always to ensure the safety of the patient and others while conducting a thorough diagnostic workup.
- Prioritize Safety: Your first step is always to assess for imminent danger. Ask directly about suicidal or homicidal ideation, intent, and plans. If a risk is identified, immediate action to create a safe environment (e.g., one-on-one observation, removing dangerous items) is the top priority.
- Rule Out Medical Causes: Always consider and rule out medical or substance-induced causes for acute psychiatric symptoms. A thorough history, physical exam, and initial labs (e.g., CBC, CMP, urinalysis, urine drug screen, TSH) are non-negotiable before settling on a primary psychiatric diagnosis. This is a common pitfall on the exam.
- Know Commitment Criteria: Understand the legal criteria for involuntary commitment (psychiatric hold). Generally, this requires the patient to be a danger to self, a danger to others, or gravely disabled (unable to provide for basic needs). Your documentation must clearly support these criteria.
Test-Taking Tip: When presented with a patient with altered mental status, never jump to a psychiatric diagnosis without first considering a medical workup. The USMLE loves to test for delirium secondary to infections, metabolic disturbances, or substance withdrawal masquerading as a primary psychiatric condition.
Mastering the approach to these challenging cases requires a blend of clinical acumen and procedural knowledge. For students looking to refine their study habits for such complex topics, exploring effective study techniques for med students can provide a significant advantage.
5. Obstetric Emergency Management
Obstetric emergencies are a critical component of the USMLE Step 3, testing your ability to manage life-threatening conditions for both mother and fetus. These high-stakes scenarios evaluate your grasp of rapid assessment, stabilization, and timely intervention in situations like severe preeclampsia, placental abruption, and postpartum hemorrhage. Questions in this domain often come in the form of challenging Computer-based Case Simulations (CCS), requiring you to not only know the textbook answers but also to execute them in a logical, time-sensitive sequence.

A classic sample USMLE Step 3 question might present a 34-week pregnant patient with a sudden spike in blood pressure to 165/115 mmHg, proteinuria, and a severe headache. You would need to diagnose severe preeclampsia, initiate magnesium sulfate for seizure prophylaxis, and decide on the appropriate antihypertensive agent and timing for delivery. Another common scenario is postpartum hemorrhage, where you must quickly identify the cause (e.g., uterine atony) and initiate sequential treatments from uterine massage and oxytocin to more invasive procedures.
Strategic Approach and Key Takeaways
Success in obstetric emergency questions depends on recognizing specific diagnostic criteria and implementing established management protocols without delay. You must quickly differentiate between various causes of third-trimester bleeding or postpartum complications, as initial steps can be life-saving.
- Preeclampsia with Severe Features: Know the criteria cold: BP ≥160/110 mmHg, thrombocytopenia, elevated liver enzymes, severe right upper quadrant pain, new-onset headache, or visual disturbances. The definitive treatment is delivery, but your first step is always maternal stabilization with magnesium sulfate and antihypertensives (labetalol, hydralazine, nifedipine).
- Postpartum Hemorrhage (PPH): Remember the "4 T's" of PPH causes: Tone (atony), Trauma (lacerations), Tissue (retained placenta), and Thrombin (coagulopathy). Your initial management should always address uterine atony first with fundal massage and uterotonic agents like oxytocin.
- Placental Abruption: Suspect this with painful vaginal bleeding, uterine tenderness, and fetal distress. Your immediate actions should be to establish two large-bore IV lines, type and crossmatch blood, and prepare for an emergency C-section if there are signs of fetal or maternal instability.
Test-Taking Tip: On CCS cases, always remember to consult OB/GYN early. However, do not wait for the consultant to arrive before initiating critical life-saving measures like administering magnesium sulfate for eclampsia or starting fluid resuscitation for hemorrhage. Your initial actions count.
This structured thinking ensures you address the most immediate threats first. Mastering these high-yield scenarios is vital, as they are a frequent source of challenging sample USMLE Step 3 questions that directly test your readiness for independent practice.
6. Infectious Disease Outbreak Investigation
Step 3 uniquely tests your grasp of public health and epidemiology, making outbreak investigations a crucial topic. These questions assess your ability to function beyond a single patient encounter and think like a systems-level physician. You must analyze population data, identify patterns, and implement measures that protect community health. Scenarios often require you to act as the primary care physician who first notices a cluster of illnesses, placing the responsibility on you to initiate the public health response.
A typical sample USMLE Step 3 question could present a scenario where several children from the same daycare present to your clinic with vomiting and diarrhea. Another might involve a cluster of post-operative surgical site infections on a single hospital ward. You would be expected to not only treat the individual patients but also report the cluster to the appropriate authorities, obtain detailed exposure histories, and suggest initial infection control measures, such as cohorting patients or reinforcing hand hygiene protocols.
Strategic Approach and Key Takeaways
Success with outbreak questions requires a shift from individual diagnosis to epidemiological thinking. You need to quickly determine the nature of the outbreak and the most likely mode of transmission to guide your next steps.
- Recognize and Report: Your first step is recognizing that an outbreak may be occurring. A key action is notifying the local or state health department. This is often a critical answer choice.
- Epidemiological Clues: Carefully analyze the "person, place, and time" data provided. Create a line list or epidemic curve in your mind. A sharp upward slope with a rapid decline suggests a common-source exposure (like contaminated food at a picnic), while a slower, progressive rise suggests person-to-person spread.
- Implement Control Measures: Based on the suspected transmission route, you must choose appropriate infection control actions. This could range from isolating patients with suspected airborne diseases to issuing a boil-water advisory for a community-wide gastrointestinal illness.
Test-Taking Tip: Pay close attention to the timeline and patient demographics. If all affected individuals ate at the same restaurant on the same day, a foodborne, common-source outbreak is almost certain. If cases are spread out over weeks among family members, think person-to-person transmission.
Understanding the physician's role in the broader public health system is a key differentiator on Step 3. These questions test your ability to protect both your individual patient and the community at large. Mastering the fundamentals of outbreak investigation is essential for demonstrating readiness for independent practice.
7. Geriatric Polypharmacy Assessment
Geriatric polypharmacy is a core competency tested on the USMLE Step 3, reflecting the growing complexity of managing elderly patients. Questions in this domain assess your ability to look beyond a single chief complaint and evaluate the patient's entire medication list for interactions, adverse effects, and appropriateness. These scenarios often involve subtle presentations, like falls or cognitive decline, that are direct consequences of a patient's drug regimen, challenging you to practice deprescribing and prioritize patient safety and quality of life.
A classic sample USMLE Step 3 question might present an 80-year-old female with a recent fall and new-onset confusion. Her medication list includes an antihypertensive, a statin, a benzodiazepine for sleep, an over-the-counter anticholinergic for allergies, and a new antibiotic for a UTI. Your task would be to identify the medications contributing to her altered mental status and fall risk, specifically the benzodiazepine and the anticholinergic, and formulate a safer management plan. Another example could involve a frail elderly patient with end-stage renal disease, requiring you to adjust medication dosages and discontinue drugs that are contraindicated.
Strategic Approach and Key Takeaways
Successfully navigating geriatric polypharmacy questions requires a meticulous and patient-centered approach. You must systematically review the medication list in the context of the patient’s comorbidities, functional status, and goals of care.
- Beers Criteria: Familiarize yourself with the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Be ready to identify high-risk drugs like anticholinergics (e.g., diphenhydramine), certain antipsychotics, benzodiazepines, and sliding-scale insulin.
- Assess the "Prescribing Cascade": Be alert for scenarios where a new drug is prescribed to treat the side effects of another medication. Your role is to identify the original offending agent and address the root cause.
- Incorporate Functional Status: The best medical decision isn't always about achieving perfect lab values. Consider the patient's quality of life, cognitive function, and fall risk when deciding to add or remove a medication.
Test-Taking Tip: When you encounter an elderly patient with nonspecific symptoms like confusion, dizziness, or falls, your first instinct should be to scrutinize the medication list. Always calculate the patient's anticholinergic burden and consider it a primary differential diagnosis.
The challenge of these questions lies in balancing evidence-based guidelines with individualized care. For those looking to improve their study efficiency for complex topics like this, you can review some effective med student time management tips.
Step 3 Sample Question Topic Comparison
| Case Title | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Acute Coronary Syndrome Management | High: multi-step diagnostics, evolving guidelines | High: ECG, biomarkers, risk scores, cardiology access | Timely differentiation and treatment reduces mortality | Adult emergency chest pain, cardiac risk assessment | Real-world clinical decisions; integrates multiple specialties |
| Pediatric Febrile Seizure Management | Medium: age-specific criteria, selective workup | Medium: clinical exam, lumbar puncture when indicated | Accurate seizure classification; risk stratification | Pediatric febrile seizures; parent counseling | Emphasizes evidence-based care and communication |
| Diabetes Mellitus Complications and Management | High: complex acute and chronic management | High: labs, insulin dosing tools, multidisciplinary care | Manage emergencies and prevent long-term complications | Diabetic emergencies; chronic complication screening | Tests acute and chronic skills; multidisciplinary |
| Psychiatric Emergency Assessment | Medium-High: subjective assessments, legal criteria | Medium: clinical interview, risk tools, legal input | Safety risk assessment; appropriate intervention | Acute psych emergencies: suicidal ideation, psychosis | Integrates legal, medical, and communication skills |
| Obstetric Emergency Management | High: rapid, multidisciplinary care | High: fetal/maternal monitoring, obstetric specialist support | Maternal and fetal stabilization; emergency delivery | Pregnancy complications: preeclampsia, hemorrhage | Involves dual-patient emergency care; high-yield |
| Infectious Disease Outbreak Investigation | Medium: epidemiological methods, reporting | Medium: public health communication, contact tracing | Identify and contain outbreaks, public health safety | Outbreaks in community or healthcare settings | Emphasizes systems-based and preventive medicine |
| Geriatric Polypharmacy Assessment | Medium-High: complex med review, functional assessment | Medium: medication review tools, cognitive tests | Optimize medications; reduce adverse events | Elderly patients with multiple comorbidities | Focuses on quality of life and drug safety |
Integrating These Strategies for Peak Exam Performance
Navigating the USMLE Step 3 is less about memorizing isolated facts and more about mastering the art of clinical reasoning under pressure. The sample USMLE Step 3 questions we have deconstructed in this article are not just practice material; they are strategic blueprints for success. Each example, from managing acute coronary syndrome to assessing geriatric polypharmacy, reveals a core pattern that the exam consistently tests: the ability to synthesize data, prioritize actions, and anticipate the next best step in patient care.
By working through these questions, you have seen firsthand how the exam weaves together foundational science with advanced clinical management. The key is to move beyond simply identifying the correct answer. The real learning happens when you dissect the why behind each choice, understanding why the distractors are incorrect for this specific clinical scenario. This deeper level of analysis is what transforms good students into exceptional test-takers.
Your Strategic Action Plan Moving Forward
To truly integrate these lessons, you must adopt a proactive and analytical approach to your remaining study time. Merely completing more questions is not enough; the quality and depth of your review are what will elevate your score.
Here are the most critical takeaways to implement immediately:
- Embrace the Two-Step Diagnosis: For every vignette, first establish the most likely diagnosis, then determine the most appropriate next step in management. As seen in the obstetric emergency and pediatric seizure questions, the diagnosis is often just the entry point to a more complex management decision.
- Prioritize, Don't Just Identify: The Step 3 exam environment mirrors real-life clinical urgency. Always ask yourself: "What is the most immediate threat to this patient's life or well-being?" This mindset, crucial for the ACS and psychiatric emergency scenarios, will help you filter out secondary or less urgent interventions.
- Master Foundational Concepts: High-yield topics like diabetes management and infectious disease principles will appear in various forms. A robust understanding of these areas allows you to adapt to novel presentations and confidently handle the unique challenges presented in Computer-based Case Simulations (CCS).
- Analyze Your Errors Systematically: Do not just read the correct answer explanation and move on. Categorize your mistakes. Was it a knowledge gap? A reading comprehension error? A failure to prioritize? Identifying these patterns is the first step to correcting them.
The value of mastering these approaches extends far beyond your exam score. The skills you are honing, such as rapid clinical assessment, evidence-based decision-making, and risk management, are the very skills that define a competent and confident physician. By practicing with challenging sample USMLE Step 3 questions and focusing on these strategic principles, you are not just preparing for a test; you are preparing for your career.
Ready to transform your preparation with a comprehensive, high-yield resource? Ace Med Boards offers an extensive Qbank filled with challenging questions and detailed explanations designed to build your clinical reasoning skills for Step 3. Elevate your study strategy and gain the confidence you need to excel by exploring our proven platform at Ace Med Boards.

