Clinical experience is your first real taste of life in healthcare. It's any hands-on learning where you're either interacting directly with patients or observing their care up close. Think of it as the essential bridge between what you read in a textbook and the dynamic, unpredictable reality of practicing medicine. For any serious medical school applicant, it's completely non-negotiable.
Understanding Clinical Experience Beyond the Dictionary Definition
Let’s reframe this. Imagine your medical education is like learning to navigate a sprawling, complex city. Your lectures and textbooks are the map—they show you the street names, the landmarks, and the basic rules of the road.
So, what is clinical experience? It’s finally getting behind the wheel. It's merging into traffic, dealing with unexpected detours, and learning to react in real-time, all with a seasoned driver guiding you. This is how abstract knowledge becomes a practical, usable skill.
This hands-on training is so much more than just logging hours for an application. It’s where you start building the core competencies that define a great physician. You'll witness the human side of medicine firsthand—grappling with patient emotions, navigating tough ethical questions, and seeing the stark realities of illness. You stop just memorizing symptoms and start learning to listen, observe, and connect.
The Core Pillars of Clinical Experience
To help you get a clearer picture, let's look at what makes for a truly meaningful clinical experience. Admissions committees are looking for evidence that your time was well-spent and that you understand what it actually means to care for people. It all boils down to three fundamental pillars.
| Component | What It Means | Real-World Example |
|---|---|---|
| Patient Interaction | This is about direct engagement. It's your chance to practice communication and empathy. | Taking a patient's medical history, measuring their vitals, or even just offering a comforting presence during a difficult moment. |
| Clinical Environment Exposure | This means understanding the healthcare ecosystem—how doctors, nurses, techs, and others collaborate. | Shadowing in a busy ER and seeing how the team communicates and triages patients under immense pressure. |
| Insight into a Physician's Role | This involves observing the diagnostic process, treatment planning, and the immense responsibility doctors carry. | Watching a physician explain a complex diagnosis to a family and seeing the blend of clinical knowledge and compassion required. |
These pillars ensure you're not just a passive observer but an active learner who is starting to internalize the demands and rewards of the profession.
The goal of clinical experience isn’t just to see medicine in action; it's to start thinking and acting like a future physician. It’s about building a foundation of empathy, professionalism, and critical thinking before you even step into medical school.
Ultimately, these experiences provide the compelling stories and genuine reflections you'll need for your applications and interviews. They prove you’ve tested your commitment to this incredibly demanding field and have started developing the personal qualities necessary to thrive.
For a deeper dive, you can explore more about gaining clinical experience for pre-med students to make sure your journey starts on solid ground. This foundational understanding is what separates a good applicant from a great one.
Distinguishing Between Direct and Indirect Patient Contact
Not all clinical hours are created equal, especially in the eyes of admissions committees and residency program directors. The biggest dividing line is between experiences with direct patient contact and those that are purely observational, often called indirect patient contact.
Getting this difference right is one of the most critical parts of building a strong, competitive application.
Think of it like learning to cook. Watching a chef is the indirect experience. You see the techniques and understand the process, but you don't feel the knife in your hand or the heat from the stove. Direct experience is when the chef hands you the ingredients and says, "Your turn," guiding you as you go. One builds knowledge; the other builds skill and proves you can handle the heat.
What Is Direct Patient Contact?
Direct patient contact means you have hands-on responsibilities where your actions genuinely affect a patient's care, comfort, or medical journey. You aren't just a fly on the wall; you're an active participant in the healthcare ecosystem.
These are the roles that show you can handle responsibility, communicate effectively under pressure, and show true empathy when it really counts.
Examples of high-value direct patient contact include:
- Medical Assistant (MA): Taking patient histories, measuring vital signs, and assisting with minor procedures.
- Emergency Medical Technician (EMT): Providing emergency care in the field, assessing patients in distress, and transporting them to the hospital.
- Certified Nursing Assistant (CNA): Helping patients with daily activities, monitoring their condition, and providing direct personal care.
- Medical Scribe: Documenting the physician-patient encounter in real-time, which demands deep engagement with the entire diagnostic and treatment process.
This flowchart shows how real patient care is built on a foundation of essential skills.
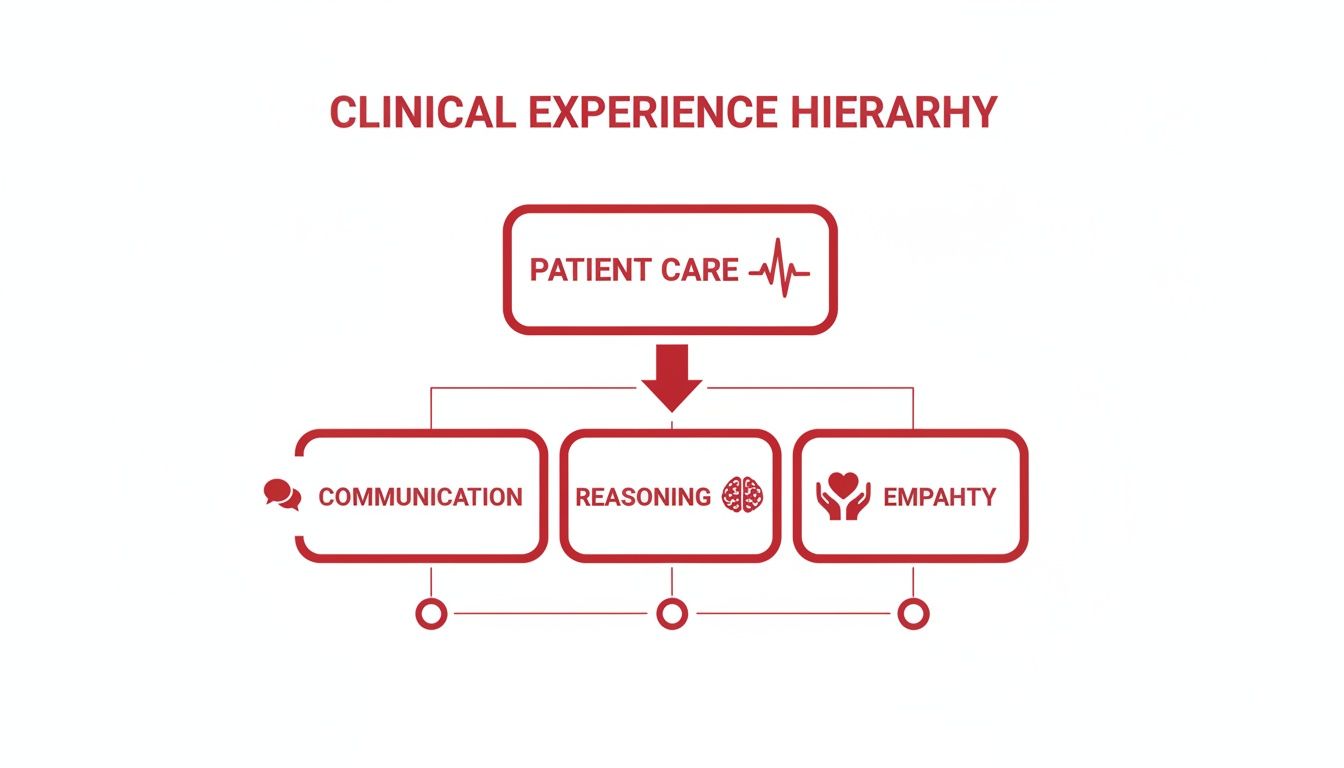
As the image shows, effective patient care isn't just one skill. It’s a mix of communication, clinical reasoning, and empathy all working together. These are the exact abilities you sharpen through direct, hands-on clinical work.
Understanding Indirect Patient Contact
Indirect patient contact, often just called shadowing or observational experience, is when you're in a clinical setting but without direct responsibility for patient care. These roles are absolutely essential for confirming your interest in medicine and getting a feel for the day-to-day grind of a physician.
While valuable, admissions committees see them as a starting point, not the end of your clinical journey.
Common examples of indirect experience are:
- Physician Shadowing: Following a doctor during their rounds or in the clinic to observe their work.
- Hospital Volunteering (Administrative): Working at an information desk, delivering flowers, or handling paperwork without patient interaction.
- Clinical Research (Data Entry): Analyzing patient data or managing study files without directly engaging with the study participants themselves.
Direct vs Indirect Clinical Experience at a Glance
To help you prioritize your efforts for medical school and residency applications, here’s a quick comparison of direct versus indirect clinical experience.
| Attribute | Direct Patient Care | Indirect/Observational Experience |
|---|---|---|
| Your Role | Active participant with defined responsibilities. | Passive observer learning from the sidelines. |
| Primary Goal | Develop and demonstrate core clinical skills. | Confirm interest and understand the medical field. |
| Impact on App | High. Shows commitment, empathy, and resilience. | Foundational. Shows you’ve done your homework. |
| Examples | EMT, CNA, Medical Assistant, Scribe. | Shadowing, hospital admin, non-interactive research. |
| Key Takeaway | Proves you have the skills and grit for patient care. | Shows you have explored the profession seriously. |
Ultimately, a strong application needs a healthy balance of both. Indirect experience shows you've done your homework, while direct experience proves you have what it takes to step into the demanding world of patient care.
This progression from observer to doer is fundamental—not just for you, but for licensed physicians, too. A doctor's clinical experience is defined by the hands-on practice they get after medical school, usually during residency. In fact, all 50 U.S. state medical boards mandate at least one year of postgraduate training for a license, with some surgical specialties requiring up to seven years. This ensures every doctor is truly ready for independent practice.
This same transition from watching to doing happens in medical school during core rotations. For a deeper dive into this critical phase of training, check out our guide on what is a clerkship. It breaks down how students finally get to apply classroom knowledge in real clinical settings—a process that starts with the foundational experiences you're gaining right now.
Why Meaningful Clinical Experience Is Your Most Valuable Asset
Thinking of clinical experience as just another box to check on your application is like saying astronaut training is just about “passing some tests.” It completely misses the point. Meaningful clinical exposure is the single best way to prove—first to yourself, and then to admissions committees—that you’re genuinely cut out for a life in medicine.
This isn’t about proving you can handle the sight of blood. It’s about showing you have the empathy, resilience, and maturity to connect with people when they are at their most vulnerable. It’s your chance to really test-drive your commitment before you dedicate the next decade of your life to this demanding path.
Confirming Your Commitment to Medicine
Reading about medicine is one thing. Living it, even for a short time, is something else entirely. Clinical experience gives you an unfiltered preview of a physician’s life: the long hours, the emotional weight, and the incredible satisfaction. It’s the ultimate reality check.
These hours in the clinic or hospital force you to answer some tough questions:
- Can you still show compassion when you're exhausted and overwhelmed?
- Do you have the emotional strength to deliver difficult news?
- Can you really function as part of a complex, fast-moving healthcare team?
Answering "yes" after seeing these things firsthand carries so much more weight than just writing it in an essay. It’s a huge part of what medical schools look for in a candidate—they want evidence of a commitment that has been tested and has proven durable.
Meaningful clinical experience is where you stop saying "I want to be a doctor" and start understanding what it truly takes to become one. It's the moment your abstract ambition gets tested by real-world human interaction.
Without this trial by fire, your motivation is purely theoretical. Admissions committees see thousands of applicants; they can easily spot the difference between someone who has romanticized the idea of being a doctor and someone who has looked the challenges squarely in the face and is still determined to move forward.
Building the Foundation for Clinical Judgment
Beyond just confirming your path, clinical experience is where you start building the most essential skill a doctor has: clinical judgment. Think of it as the ability to connect the dots between textbook knowledge, a patient's story, and subtle clues you pick up just by observing. It’s a skill that absolutely cannot be learned from a book.
Every patient encounter you have—whether you're taking vitals as a CNA or documenting a history as a scribe—is training your brain to think like a physician. You start recognizing patterns, asking sharper questions, and understanding the subtle art of patient communication.
This foundation becomes priceless when you're staring down high-stakes board exams. Success on the USMLE Step 2 CK and COMLEX Level 2 isn't about rote memorization; it's about working through complex clinical vignettes that are designed to test your clinical reasoning.
For instance, a question might give you a patient with vague symptoms and ask for the "next best step." Your ability to nail that question comes directly from having seen similar situations play out in a real clinic. You’ll remember how a physician triaged a similar case, what questions they asked, and why they ordered one test over another. This real-world context turns abstract facts into a practical, problem-solving toolkit. The more scenarios you’ve seen, the bigger your mental library of cases becomes, giving you a massive advantage on exam day. Those hands-on hours are a direct investment in your future board scores.
How to Find High-Impact Clinical Opportunities
Knowing what clinical experience is and why it matters is one thing, but turning that knowledge into action is the real challenge. You need to be proactive and strategic to land the kinds of opportunities that let you move from a passive observer to an active participant in patient care.
These experiences are your training ground. They're where you'll build the skills and find the stories that make your medical school application truly compelling. Let’s get into the practical ways to find them.

Start with Traditional and Paid Roles
Some of the best, most impactful clinical experiences come from established, paid positions that put you right in the middle of a healthcare setting. These roles often require some sort of certification, but the hands-on responsibility you get is second to none.
Consider these powerful options:
- Medical Assistant (MA): This role is all about direct patient contact. You'll be taking vitals, recording patient histories, and even assisting with minor procedures.
- Emergency Medical Technician (EMT): As an EMT, you’re on the front lines. It’s intense, high-stakes work providing immediate care, but it’s an incredibly formative experience.
- Certified Nursing Assistant (CNA): Working as a CNA gives you a deep understanding of long-term patient care and the daily needs of vulnerable populations in hospitals or nursing homes.
- Medical Scribe: Scribing puts you shoulder-to-shoulder with a physician, documenting patient encounters in real-time. You get a front-row seat to their diagnostic process and clinical decision-making.
If you're serious about landing one of these roles, it's worth studying successful resume examples for Medical Assistant roles to make your application stand out.
Leverage Your Network and Academic Connections
Don't underestimate the power of the people around you. Your university and local community are packed with opportunities that you won't find advertised online.
Start with your pre-health advisor. They usually have established relationships with local hospitals, clinics, and physicians who are open to taking on students. Also, make a point to talk to your science professors; many have colleagues in clinical research or private practice who might need a dedicated student for a project or observation.
Think of networking as building bridges. Every conversation with a professor, physician, or even an older student can lead to an opportunity that shapes your entire medical journey.
This personal approach often leads to far more unique and meaningful experiences than just applying to a generic volunteer program. You can find more specific advice in our complete guide on how to get clinical experience.
Special Considerations for International Medical Graduates
For International Medical Graduates (IMGs), getting U.S. clinical experience (USCE) isn't just a good idea—it's a critical step toward residency. This experience proves you're familiar with the U.S. healthcare system, its protocols, and its standards of patient care. The biggest hurdle is often finding institutions willing to host IMGs.
Focus your energy on a few key strategies:
- Utilize Placement Agencies: There are many organizations out there that specialize in connecting IMGs with U.S. hospitals for hands-on externships and observerships.
- Network with IMG Alumni: Reach out to graduates from your medical school who have successfully matched into U.S. residencies. They can offer priceless advice and may have contacts to share.
- Cold Emailing and Calling: It might feel like a long shot, but directly contacting physicians and program coordinators at smaller community hospitals can work. They often have more flexibility than large academic centers.
This process is so important because USCE is a cornerstone of the licensing pathway for physicians trained outside the U.S. While 41 of 50 states traditionally require a U.S. or Canadian residency, some are creating new pathways. Alabama, for instance, now allows IMGs with three years of recent experience abroad to get a temporary license after passing state boards, bypassing the residency requirement.
By pursuing these different avenues, you can build a strong, compelling portfolio of clinical experiences that will not only make your application stand out but also prepare you for the realities of medical training.
Turning Your Clinical Hours Into Compelling Stories
Let's be honest. Just logging a ton of hours in a clinic won't get you into medical school. It's a start, but it's not the whole game. Admissions committees aren't impressed by a number on a page; they're looking for the quality of your reflection. Your real job is to transform those hours into powerful stories that show them who you are—your empathy, your growth, and your fitness for a life in medicine.
This isn't something you do the night before your application is due. It starts the moment you walk into the clinic. You have to shift your mindset from being a passive observer to an active, thoughtful participant. This is where you start connecting what you see day-to-day with the bigger picture of what it truly means to be a doctor.

From Observation to Insightful Reflection
Your most powerful tool in this process? A simple reflection journal. This isn't just a logbook of tasks you completed. Think of it as a space to unpack your experiences, process your emotions, and pinpoint the lessons you're learning. Trust me, the specific details of a powerful patient encounter can fade incredibly fast, so writing them down is critical.
After every shift, just take ten minutes. Jot down your thoughts about what stood out. If you're stuck, use these prompts to get started:
- What was the toughest patient interaction I had today, and why? This helps you really dig into your communication skills and emotional grit.
- Did I witness a tricky ethical situation? Thinking through these moments shows you can handle the gray areas of medicine.
- What did I learn from watching the healthcare team work together? This shows you get that modern medicine is a team sport.
- How did a specific patient's story affect me personally? This is where you find the moments that built your empathy.
This habit turns vague experiences into a bank of concrete examples you can pull from for essays and interviews. It’s the raw material you'll use to build a narrative that proves you belong in medicine.
Your ability to reflect on your clinical experience and articulate what you've learned is more impressive to an admissions committee than the number of hours you’ve accumulated. They want to see evidence of growth and self-awareness.
The Art of Showing, Not Telling
You've probably heard the advice "show, don't tell" a thousand times. But what does that actually mean for your med school application? It means using specific stories to prove you have the qualities of a future physician, rather than just claiming you have them.
Don't just write, "I am an empathetic person." Instead, describe the time you sat with a frightened patient, what you said, and what that taught you about the human side of care. Don't state, "I am resilient." Tell the story of a chaotic day in the ER and how you navigated the emotional weight while staying focused. This approach makes your claims believable and, more importantly, memorable.
To really nail this, you need to connect your experiences back to the core competencies of medicine. For instance, a story about helping a non-English-speaking patient navigate the clinic showcases your cultural competency and problem-solving skills. A story about witnessing a physician work through a complex diagnosis highlights your intellectual curiosity. Building these narratives is a crucial step, and using a structured tool like a personal statement outline can be a huge help in organizing your best stories.
By making a conscious effort to reflect on your clinical hours and shape them into powerful narratives, you create an application that tells the compelling story of a future physician in the making. That's how you prove you have the maturity and insight to succeed.
Translating Clinical Skills Into Board Exam Success
All those hours you spend in the hospital and clinic aren't just a box to check for applications. They’re your secret weapon for crushing high-stakes board exams like the USMLE and COMLEX. These tests aren't really about regurgitating facts from a textbook; they're designed to see how well you think like a doctor. In other words, they test your clinical reasoning—the very skill you’re sharpening with every patient you see.
Think of it like this: your preclinical years give you all the raw ingredients of medical knowledge. It's during your clinical rotations that you actually learn how to cook. You figure out how to combine those ingredients, adjust when things don't go as planned, and ultimately create a successful outcome for your patient. Board exams are the final test—they hand you a new set of ingredients and ask, "Alright, show us what you can make."
From the Bedside to the Test Center
Every challenging patient you encounter is basically a live-action board exam question. That complex differential diagnosis you struggled through on your Internal Medicine rotation? That’s a classic USMLE Step 2 CK vignette waiting to happen. The time you had to decide the next best step for a pediatric patient with a fever? That’s a core competency you'll see on your Shelf exams.
This direct, hands-on experience builds an intuitive understanding that rote memorization just can't touch. When you read a case-based question, your brain won't just be scanning a database of facts. It will pull up memories of real people—the sights, the sounds, the gut feelings, and the critical decisions your team made. This context is what helps you slice through the noise and pinpoint the most important details, a make-or-break skill on test day.
Why Hands-On Experience Outperforms Memorization
Board questions are intentionally structured to mirror real-world clinical decision-making. They’re testing your ability to synthesize information, recognize patterns, and prioritize what to do next, all under pressure. This is precisely where your clinical experience pays off big time.
Think about the direct connections:
- Internal Medicine Rotations: These directly prep you for questions on complex adult diseases, tricky pharmacology, and diagnostic puzzles.
- Surgery Rotations: This is where you solidify your knowledge of anatomy, pre- and post-op care, and how to spot a surgical emergency from a mile away.
- Pediatrics Rotations: You get the real-world reps needed to confidently tackle questions on developmental milestones, congenital conditions, and unique pediatric illnesses.
Your time in the clinic provides a mental library of patient stories. On exam day, you're not just answering a question; you're recalling a real-life scenario and applying the lessons you learned at the bedside.
Unfortunately, the system doesn't always value this experience equally. International Medical Graduates (IMGs), who often have incredibly rich hands-on training, can face frustrating biases. Data from the U.S. shows IMGs frequently have more clinical experience than their domestic peers but still face lower residency match rates. In Canada, the gap is even more stark: less than 50% of IMGs pass their certification OSCEs, compared to 93.5% of domestic graduates, a number that highlights major challenges in how real-world skills are assessed. You can learn more about these findings on physician assessment.
This is where smart, dedicated preparation becomes essential. Services like Ace Med Boards help you synthesize all that hands-on knowledge and turn it into a concrete strategy for exam day. Expert tutoring can bridge the gap between what you did in the clinic and how to prove you know it on the test, making sure your hard-earned skills translate into a score that reflects your true abilities.
Common Questions About Clinical Experience
As you start piecing together your path to medical school, you’re bound to have questions about clinical experience. It's one of the most talked-about parts of an application, and the expectations can feel a bit murky. Let's clear up some of the most common questions students ask so you can build your application with confidence.
How Many Clinical Hours Do I Truly Need?
There’s no magic number that opens the door to an acceptance letter, but a good rule of thumb is to aim for over 100 hours. That said, admissions committees will always, always choose quality over quantity.
A long-term commitment to one or two roles is far more impressive than a dozen short-lived activities. When you stick with a position, you get to show growth, take on more responsibility, and form real connections. Focus on deep, meaningful engagement, not just checking off a box.
Does Paid Clinical Work Look Better Than Volunteering?
Admissions committees see value in both, because they each tell a different part of your story. A paid job, like being an EMT or a medical scribe, shows that you can handle responsibility and succeed in a professional healthcare setting. It proves you have stamina and real-world skills.
On the other hand, volunteering—especially with underserved communities—screams altruism and a genuine desire to serve. The best strategy? Go for the opportunities you're truly passionate about, paid or not, as long as they involve significant patient interaction.
The real question isn't whether you got a paycheck; it's what you got out of the experience. A powerful, reflective story about a single patient you met while volunteering can carry more weight than hundreds of paid hours you can't talk about thoughtfully.
Is Shadowing a Doctor Direct Clinical Experience?
Nope. Shadowing is a critical observational experience, but it’s not direct patient care. It's incredibly valuable for getting a realistic peek into a physician's daily life, confirming that this is the career for you.
But because you aren’t hands-on—you're not taking vitals, talking to patients on your own, or performing any duties—it doesn't count as direct experience. A strong application needs a healthy mix of both: shadowing to show you've explored the profession, and direct patient care to prove you can handle being a part of it.
What If My Access to Opportunities Is Limited?
Admissions committees get it. They know that your ability to find clinical roles can depend heavily on where you live and your personal situation. If you're in a rural area or have other constraints, don't panic.
Focus on making the most of what is available. Even a single, long-term role can be incredibly powerful if you can speak about it with insight and passion. Talk about what you learned, how you grew, and how it solidified your decision to pursue medicine. You can also round out your application with other service-oriented activities that showcase your empathy and dedication to helping people—and you can always briefly explain any limitations in your application.
Ready to connect your clinical experience to top-tier board scores? At Ace Med Boards, our expert tutors help you translate that hands-on knowledge into high-stakes exam performance. Visit https://acemedboards.com to schedule a free consultation and build your winning strategy.
