Receiving a failing score on USMLE Step 3 is a gut punch. There's no other way to put it. But it is absolutely a recoverable setback, not a career-ender. The most critical thing you can do right now is take measured, strategic action within the first 48 hours.
Your immediate game plan should be simple: inform your program director, get your hands on your performance report, and then—this is important—give yourself a planned break to mentally reset.
Your First Steps After a Failed Step 3
That moment you see a non-passing score can feel like the world is ending. It's a genuine shock, especially after you've successfully cleared every single academic hurdle thrown at you until now. But how you react in these first few hours will set the stage for your comeback.
That old saying about only needing a “Number 2 pencil for Step 3” is dangerously wrong. This exam demands serious respect and preparation, and your first step is to treat this situation with the gravity it deserves.
Have the Tough Conversation First
Your absolute first priority is communication. You have to tell your residency program director (PD) what happened. This is going to be a difficult conversation, no doubt about it, but being transparent is non-negotiable for your career and for figuring out your next move within the program.
Trust me, most PDs have been through this exact scenario with other residents. They can be your biggest ally, offering guidance and helping you navigate the institutional support available.
Get Your Hands on the Performance Report
Next, shift your focus to the administrative stuff. You need to download your USMLE performance feedback report immediately. This document is everything. It's not just a score; it's the blueprint for how you're going to succeed next time.
It will show you exactly where you stumbled. Was it a knowledge deficit in Foundational Independent Practice (FIP)? Maybe you ran out of time in Advanced Clinical Medicine (ACM), or your strategy on the Computer-based Case Simulations (CCS) was flawed. This report has the objective data you need to build a smarter, more targeted study plan.
Your score report is the single most important piece of data you have. Don't waste time guessing why you failed. Let the report be your guide and show you exactly where to focus for your retake.
Why You Need to Take a Deliberate Pause
Once you've talked to your PD and have your report, the next best move feels completely counterintuitive: take a break. I'm not talking about ignoring what happened. I'm talking about giving yourself a full 24-48 hours to process the disappointment without even thinking about opening a book.
This short, intentional pause is crucial. It stops you from burning out before you even start and lets you approach your retake prep with a clear, focused mind, not one clouded by anxiety and frustration. Making a good decision about when to take Step 3 for your retake is critical, and you can't do that with a panicked mindset.
Failing is tough, but a little perspective from the data can help. While first-time pass rates are high, repeat takers have a tougher climb. Success rates for retakes hover around 76-77% for US/Canadian graduates and 64% for international medical graduates. This just underscores how important it is to have a completely new—and more effective—strategy this time around.
Your comeback doesn't start with studying more; it starts with studying differently. These initial steps are what lay that strong foundation.
Deconstructing Your Score Report to Find Weaknesses
To succeed on your retake, you have to study smarter, not just harder. That whole process kicks off with a forensic analysis of your last attempt. Your USMLE score report is the single most valuable piece of evidence you have—it’s a data-driven map showing exactly where things went sideways. Getting past the sting of seeing "fail" is the first step toward building a comeback strategy.
This is your chance to be brutally honest with yourself and diagnose the real problem. Was it a specific knowledge gap? Did you run out of steam on long question blocks? Or was it a fundamental misunderstanding of the unique Computer-based Case Simulations (CCS) format? Your report has the answers, but you need to know how to read it.
The visual decision tree below outlines the critical first moves after getting your score, leading right into the diagnostic process we’re talking about here.
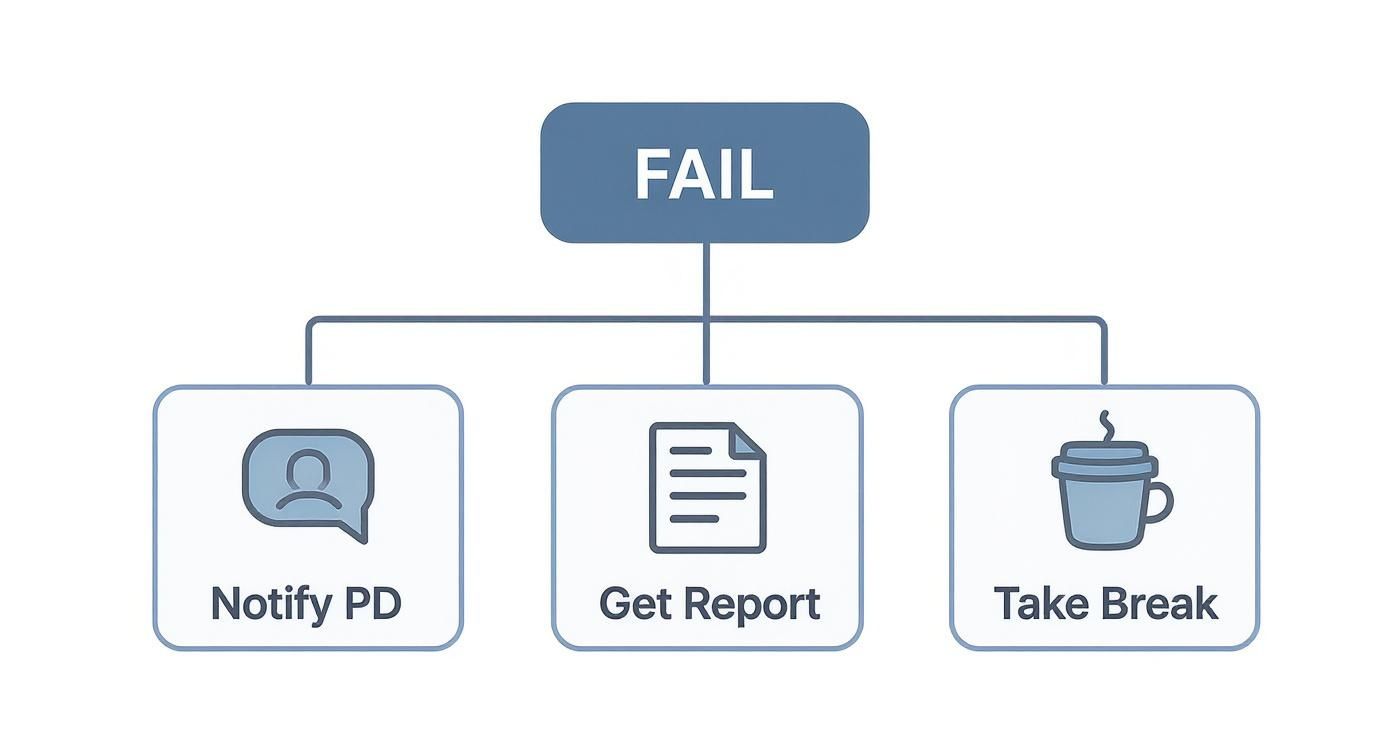
As you can see, getting that performance report is a core part of your immediate action plan. It sets the stage for an informed, targeted study approach that actually works.
Reading Between the Lines of Your Performance Graph
The performance feedback graph is your starting point. It breaks down your performance by physician task and discipline, showing where you landed relative to the passing standard. Zero in on the bars that fall significantly below that line. These are your red flags—the high-yield areas that need immediate attention.
Don't just glance at it. Print it out. Get a highlighter and mark every single area labeled as "Lower" or "Borderline." These aren't just topics to casually review; they represent foundational weaknesses that likely cost you points across multiple questions.
For example, a low score in "Diagnosis" might mean you struggle with interpreting initial patient data. A weakness in "Health Maintenance/Epidemiology/Biostats" is a huge signal that you need to dedicate serious time to these often-neglected but heavily tested subjects.
Identifying Your True Weakness Category
Once you've flagged the low-performing content areas, the next job is to figure out the type of mistake you were making. You need to get to the "why" behind the wrong answers. Was it a knowledge gap, a strategy flaw, or an execution error?
Categorizing Your Weaknesses
| Category | Description | Example Scenario |
|---|---|---|
| Knowledge Gaps | You flat-out did not know the required medical information. | Consistently getting nephrotic vs. nephritic syndrome questions wrong because you can't recall the key differentiating features. |
| Strategy Flaws | You knew the material but applied it wrong or mismanaged your time. | Spending ten minutes on a single, complex biostats question, then having to rush through the last five questions in the block. |
| Execution Errors | Simple mistakes made because of anxiety, fatigue, or just misreading the question. | Picking the wrong answer for a drug's side effect—even though you knew the right one—because you read "most likely" as "least likely." |
Understanding these categories is everything. A knowledge gap needs focused content review. A strategy flaw, on the other hand, requires timed practice and a whole new approach to tackling question blocks.
Self-assessment is brutal but necessary. Be radically honest with yourself. Admitting that you consistently mismanaged your time or panicked during CCS cases is the first step to fixing the problem for good.
The CCS Cases: An Unforgiving Format
For a lot of people who fail Step 3, the CCS cases are the main culprit. This section makes up roughly 25% of your final score, and its unique, interactive format can be absolutely unforgiving if you haven't mastered the software and the rhythm of managing a patient.
Your score report will give you a sense of how you did here. If your performance was low, it's a five-alarm fire you need to put out. Were you ending cases early? Did you forget key follow-up orders or preventative care? These are common and costly pitfalls.
To build a stronger foundation, it’s worth reviewing the official USMLE content outline to make sure your study plan is perfectly aligned with the exam's structure, especially for the high-yield topics that pop up constantly in CCS cases.
This detailed teardown of your prior attempt isn't about dwelling on the past. It's about gathering the intel you need to build a targeted, efficient, and ultimately successful study plan for your retake. This diagnostic work ensures every single hour you study is aimed directly at your weakest points.
Building Your High-Yield Retake Resource Stack
Let’s be blunt: using the exact same study materials that led to a failing score is a recipe for a repeat performance. A successful retake after you failed USMLE Step 3 demands a completely fresh, strategic look at your resources. It's time to audit your old stack, be ruthless about what didn't work, and build a new one focused entirely on fixing your specific weak spots.
Your first attempt might have been about covering everything. Now, your mission is surgical precision. Every single resource you choose must serve a distinct purpose directly tied to the weaknesses staring back at you from your score report.
Your Qbank Is Non-Negotiable, But Your Strategy Must Change
A top-tier question bank like UWorld is the bedrock of any Step 3 prep, but for a retake, you have to use it differently. Simply resetting it and grinding through thousands of questions again isn’t a strategy—it’s just repetition. Your new approach has to be diagnostic.
Instead of hitting "random," create custom, timed tests that only target the subjects where your performance was marked "Lower" or "Borderline." If your report flagged Biostatistics and Epidemiology, for instance, your first couple of weeks should be filled with daily blocks of just those questions. No hiding.
This forces you to confront your weak points head-on. You should be spending twice as long reviewing the explanations for your incorrects as you do answering the questions. Make flashcards. Write out concepts you repeatedly miss. Our guide on USMLE Step 3 practice questions dives deeper into these kinds of high-impact Qbank techniques.
Taming the Unforgiving CCS Case Format
For many residents, the Computer-based Case Simulations (CCS) are the primary reason they failed. This section makes up roughly 25% of your total grade, and your comfort level with the software and the rhythm of case management is just as crucial as your medical knowledge. You can't learn this passively.
You need a dedicated tool like CCSCases.com. The goal isn't just to "do" the cases; it's to master their logic and flow.
- Practice with Intent: Work through every single high-yield case. After each one, pull up the "expert" solution and meticulously compare it to your own. Pinpoint every order you missed or every diagnostic step you took too late.
- Develop a Rhythm: Create a standardized mental checklist for every patient encounter: history, physical, initial orders, reassessment. This prevents you from forgetting critical, easy-to-miss steps like "counsel patient" or "order vaccines" when the pressure is on.
- Master the Clock: Get comfortable with the 2-minute and end-of-case warnings. Practice placing your final orders efficiently so you never leave points on the table by ending a case prematurely.
Choosing Your Supplemental Resources Wisely
Beyond your Qbank and CCS practice, you need to be extremely selective. Piling on more resources without a clear purpose just creates noise and wastes precious study time.
First, you need a system to keep your new insights organized. Explore some knowledge management best practices to make sure your notes are streamlined and actually useful for review.
Now, only consider these additions if they directly address a need:
- Video Lectures (e.g., Boards and Beyond, OnlineMedEd): Use these only for targeted remediation. If your score report flagged Cardiology, watching that video series can help rebuild your foundational knowledge before you dive back into Qbank questions on the topic.
- Review Books (e.g., First Aid for Step 3, Master the Boards): These should function as reference tools, not primary study materials. Use them to look up specific details you got wrong in a practice question, not for page-by-page passive reading.
- Personalized Tutoring: If you're genuinely struggling to identify why you're making mistakes or need help crafting a better test-taking strategy, a tutor can be a game-changer. This is a high-impact option for anyone feeling truly stuck.
Here's some important context. While first-time takers from US MD programs have a pass rate of about 97%, the rate for repeat attempts among International Medical Graduates (IMGs) is around 64%. This data isn't meant to discourage you; it's meant to underscore why a generic approach won't cut it and why your resource stack must be highly effective and personalized.
To help you decide what you need for your retake, here's a quick comparison of the most common resources.
Comparison of Key USMLE Step 3 Retake Resources
This table compares the primary features, ideal use cases, and focus areas of the top study resources to help you build an effective study plan for your retake.
| Resource | Primary Focus | Best For | Key Feature for Retakers |
|---|---|---|---|
| UWorld Qbank | MCQ Practice & Content Review | Everyone, but essential for identifying and targeting knowledge gaps. | Creating custom, timed blocks focused exclusively on weak subject areas. |
| CCSCases.com | CCS Case Simulation Practice | Candidates who scored low on the CCS portion or feel uncomfortable with the format. | Direct comparison of your performance against an "expert" solution to refine case management. |
| Boards and Beyond | Foundational Science & Clinical Knowledge | Rebuilding a weak knowledge base in a specific subject before tackling questions. | In-depth video explanations that connect basic science to clinical presentation. |
| OnlineMedEd | Clinical Reasoning & Frameworks | Solidifying a structured approach to common clinical problems. | Provides easy-to-remember frameworks for diagnosis and management. |
| First Aid/Master the Boards | Quick Reference | Looking up specific facts or algorithms after identifying a gap in a practice question. | High-yield fact repository; not for primary learning. |
| Personalized Tutoring | Strategy & Personalized Feedback | Candidates struggling with test anxiety, timing, or identifying error patterns. | One-on-one guidance to deconstruct your thought process and fix systemic issues. |
Ultimately, choosing the right combination of these tools is about being honest about what went wrong the first time and picking the resources that directly fix those problems.
A common mistake is simply buying more resources. The key to a successful retake isn't the quantity of your materials but the quality of your engagement with a select, high-yield few. Your goal is mastery, not exposure.
Creating a Realistic Study Schedule During Residency
Let’s be honest: trying to study for a Step 3 retake while navigating the chaos of residency is one of the toughest challenges you'll face. The generic, one-size-fits-all study plans you find online are completely useless when you're dealing with a 28-hour call shift or the sheer exhaustion that comes with the job.
You have to shift your entire mindset. Forget about planning those mythical eight-hour study marathons on your day off. They almost never happen, and trying to force them is a fast track to burnout. Instead, success is built in the small, consistent pockets of time you can realistically carve out each day. Your schedule needs to be flexible, resilient, and laser-focused on active learning—not just passively rereading facts.
The stakes are high. Passing Step 3 is a non-negotiable requirement for medical licensure, and you only get a total of four attempts. With a retest fee of $925, failing again adds a massive financial and psychological weight. For a deeper dive into these implications, you can explore the AMA's FAQ on Step 3.

Map Your Rotations First
Before you do anything else, pull up your residency schedule for the next three to six months. You need to get brutally honest about which rotations are "heavy" and which are "light." An outpatient clinic month is a world away from a brutal inpatient ICU block.
Heavy Rotations (ICU, Surgery, Inpatient Wards): During these months, your goal is simple: maintenance. Aim for small, achievable targets just to keep the material from getting stale. This could be as simple as doing and reviewing 10-15 Qbank questions a day or running through one CCS case before you pass out. The point is consistency, not volume.
Lighter Rotations (Outpatient, Research, Electives): This is your primetime. These are the golden opportunities to make huge leaps in your prep. Block out longer, dedicated study periods here to knock out full 40-question timed blocks, review several CCS cases at a time, and take your full-length practice exams.
Build Your Schedule with Micro-Goals
Once your rotations are mapped, it's time to break down your massive study goal into tiny, actionable "micro-goals." This is how you turn a vague objective like "study cardiology" into a concrete task you can actually check off a list. The psychological boost you get from hitting these small targets day after day is a powerful motivator.
Some residents find it helpful to structure their plans using layouts similar to professional development plan templates to organize study goals alongside clinical duties.
Here’s what a week of micro-goals might look like on a lighter rotation:
- Monday: Knock out a 40-question UWorld block (timed) and review it thoroughly.
- Tuesday: Practice 3 interactive cases on CCSCases.com. Really focus on your timing and final two-minute orders.
- Wednesday: Deep dive into Biostats. Watch a few review videos, then do 20 Biostats-only questions to solidify the concepts.
- Thursday: Do another 40-question UWorld block, but this time in untimed tutor mode to focus on learning.
- Friday: Review every single incorrect question from the week. Make flashcards for the concepts you truly didn't know.
- Saturday: Time for a full-length UWSA or NBME practice exam.
- Sunday: REST. Seriously. This is non-negotiable if you want to avoid burning out.
Schedule Your Practice Exams Strategically
Practice exams like the NBME CCMSA and the UWorld Self-Assessments (UWSA) are your most critical checkpoints. They do two things perfectly: build your stamina for the grueling two-day exam format and give you the most accurate snapshot of your progress. Don't hoard them until the end.
A huge pitfall is avoiding practice tests because you're scared of seeing another bad score. You have to reframe this. These exams are diagnostic tools, not judgments. They show you exactly where the cracks are so you can fix them.
Plan to take one full-length assessment every 3-4 weeks. Schedule it on a day off and simulate the real thing as closely as possible—start early, take timed breaks, and push through the fatigue. Use the detailed results to ruthlessly hunt down your weaknesses and adjust your study plan accordingly. This isn't just about studying; it's about actively improving, week by week.
Developing Your Test Day Game Plan and Mindset

You've put in months of targeted prep. Now, your success on the Step 3 retake comes down to pure execution. This two-day marathon is as much a test of mental stamina and strategy as it is of your medical knowledge. For anyone who has failed USMLE Step 3 before, wrestling with test anxiety is a huge part of the battle.
This is where you build your armor. A clear, actionable game plan for exam day itself turns that free-floating anxiety into focused, productive energy. The goal isn't just to walk in knowing the material, but to walk in knowing exactly how you’ll handle the pressure, manage your clock, and stay sharp from the first question to the final case.
Mastering the Final Week and Night Before
The last seven days before your exam are not the time to cram new information. Think of it as your "taper" week. You're shifting from intense learning to consolidation, mental prep, and physical readiness. Overloading your brain now is a surefire way to show up fatigued and anxious on test day.
Your entire focus should be on light review and building confidence.
- Light Review Only: Stick to your flashcards, go over incorrects from your last practice test, or skim high-yield charts. The last thing you want to do is tackle a dense, new topic that could shake your confidence.
- Logistics Check: A few days beforehand, do a dry run to the Prometric center if you can. Figure out exactly how long the drive takes, where you'll park, and what the check-in process feels like. This removes a massive source of day-of stress.
- Nutrition and Hydration: In the final three days, prioritize clean eating and stay well-hydrated. Ditch the heavy, greasy foods or excessive caffeine that can mess with your sleep cycle.
The night before the exam is sacred. Protect your sleep at all costs. Put your phone away, close the books, and do something genuinely relaxing. Whether it's watching a movie, listening to music, or some light stretching, your only job is to get your mind and body rested.
The biggest mistake you can make is pulling an all-nighter. A well-rested brain's ability to recall information and reason through complex questions far outweighs any last-minute facts you might cram. Aim for 7-8 hours of solid sleep.
An Action Plan for Breaks and Between Days
Your break time is a strategic tool, not just a chance to stretch. How you use your allotted time during each block—and especially during the critical period between Day 1 and Day 2—can make or break your performance.
Have a plan for every single break. You need to know exactly what you’re going to eat and drink. Pack light, high-energy snacks like nuts, a protein bar, or fruit, and avoid sugary stuff that will lead to an energy crash. Use a few minutes for the restroom, a few to eat, and a few for a quick mental reset like deep breathing.
More importantly, you need a strict "no post-game analysis" rule. Do not look up answers during breaks. Don't text friends about specific questions. It only fuels anxiety and serves absolutely no purpose. What's done is done; your focus has to be entirely on the next block.
After Day 1, your mission is to completely disconnect. Do not open a single study resource. Go home, eat a good meal, and do something totally unrelated to medicine. You have to recharge your mental battery for the CCS cases on Day 2.
Staying Grounded at the Testing Center
The testing center itself can be a source of stress. The dead silence, the ticking clock, the other test-takers—it can all feel incredibly overwhelming. This is where simple mindfulness techniques become your secret weapon.
If you feel panic setting in during a tough block of questions, try this simple grounding exercise:
- Stop and Breathe: Close your eyes for just 10 seconds. Take one slow, deep breath in through your nose and let it out through your mouth.
- Acknowledge the Feeling: Silently tell yourself, "This is just anxiety. It's a normal response, and it will pass."
- Engage Your Senses: Plant both feet firmly on the floor. Feel the texture of your mouse or the cool surface of the desk. This simple action pulls your attention back to the present moment and away from spiraling thoughts.
This entire process takes less than 30 seconds, but it's remarkably effective at breaking the anxiety cycle and letting you re-engage with the question with a much clearer head.
Finally, know when to guess and move on. Wasting five minutes on a single question you're stuck on is a terrible strategy. It just steals time and mental energy from questions you can answer correctly. Set a hard personal limit—if you can't narrow it down after 90 seconds, pick your best guess, flag it, and move forward. Your goal is to finish every single block, and aggressive time management is the only way to make that happen.
Common Questions About Retaking Step 3
Failing Step 3 brings a flood of questions, and not just about study plans. You're probably wrestling with the administrative side of things, worrying about your career, and just trying to figure out what this means for your future. Let's cut through the noise and get you the straightforward answers you need.
This is the practical stuff—the rules, the timelines, and the real-world impact. Getting a handle on these details is the first step to moving forward with a clear head.
How Soon Can I Retake the Exam?
This is always the first question, and for good reason. According to the official USMLE rules, you have to wait until after the score for your last attempt is released before you can even reapply. From there, specific waiting periods kick in.
- You can take Step 3 up to three times within any 12-month window.
- Your fourth attempt (and any after that) has to be at least 12 months after your first try, and at least six months after your most recent one.
It’s tempting to jump back in as quickly as possible, but that's a classic mistake. Rushing a retake without fixing the root cause of the problem is a recipe for another failure. Most residents realistically need a solid three to six months to regroup, reassess, and prepare effectively.
How Many Times Can I Take Step 3?
The USMLE program is very clear on this: you get a maximum of four attempts to pass Step 3. That’s it. If you don't pass within those four tries, you become ineligible to retake the exam.
This rule really raises the stakes for every single attempt. Your second or third try can't just be a repeat of your first effort with a little more cramming. It demands a completely new, smarter strategy.
The four-attempt limit is a hard stop, not a suggestion. This is exactly why a deep, honest self-assessment after a failure is non-negotiable. You have to build your next attempt on a foundation of real, measurable improvement.
Will a Failed Step 3 Affect My Fellowship Application?
Let's be direct: it can. While Step 1 is now pass/fail, your Step 3 score is still a three-digit number that programs see. A passing score is what matters most, but hyper-competitive fellowships will absolutely scrutinize an applicant's entire exam history.
But a single failed attempt is rarely a deal-breaker, especially if you come back with a much-improved score on the retake. Program directors are often far more interested in your clinical skills, your research, and what your letters of recommendation say about you.
The key is how you handle it. If it comes up in an interview, don't be defensive. Frame it as a learning experience that forced you to become more resilient and develop better study habits. Own it, show you grew from it, and move on.
What Is the Minimum Passing Score for Step 3?
As of 2024, the magic number you need to hit is 200. This score is a composite of your performance across both days of the exam, combining the multiple-choice questions with the Computer-based Case Simulations (CCS).
Don't forget that the CCS cases are a huge part of your final grade, making up about 25% of your total score. A strong showing on the cases can be a massive boost, potentially saving you if you had a tough time on some of the multiple-choice blocks. This is precisely why dedicating serious time to CCS practice is one of the highest-yield things you can do for a retake.
Knowing the answers to these questions helps clear the fog. It lets you stop worrying about the "what ifs" and start focusing your energy where it actually counts: building a bulletproof study plan to make sure your next attempt is your last.
If you're feeling stuck and need a personalized game plan, Ace Med Boards is here to help. Our tutors specialize in guiding residents through the Step 3 retake process, helping you identify your weaknesses and build the skills to pass with confidence. Learn more and book a free consultation.
